The most common cause of knee joint damage is osteoarthritis, though it can also be the result of rheumatoid arthritis, injury, or other joint conditions. This surgery is typically considered when:
- Pain is constant and cannot be controlled with medication or other non-surgical treatments
- Daily activities such as walking, climbing stairs, or even resting are affected
- Other treatments like physical therapy or injections have not provided relief
- Stiffness and limited range of motion make it difficult to perform everyday tasks
Knee replacement is most commonly performed in individuals aged 60 or older. However, younger individuals may also undergo the procedure if their knee problems are severe and other options have been exhausted. Click below to read more about arthritis of the knee as a condition, a guide to help you make a decision about your treatment and advice on what to do while waiting for surgery if chosen.
What the surgery involves
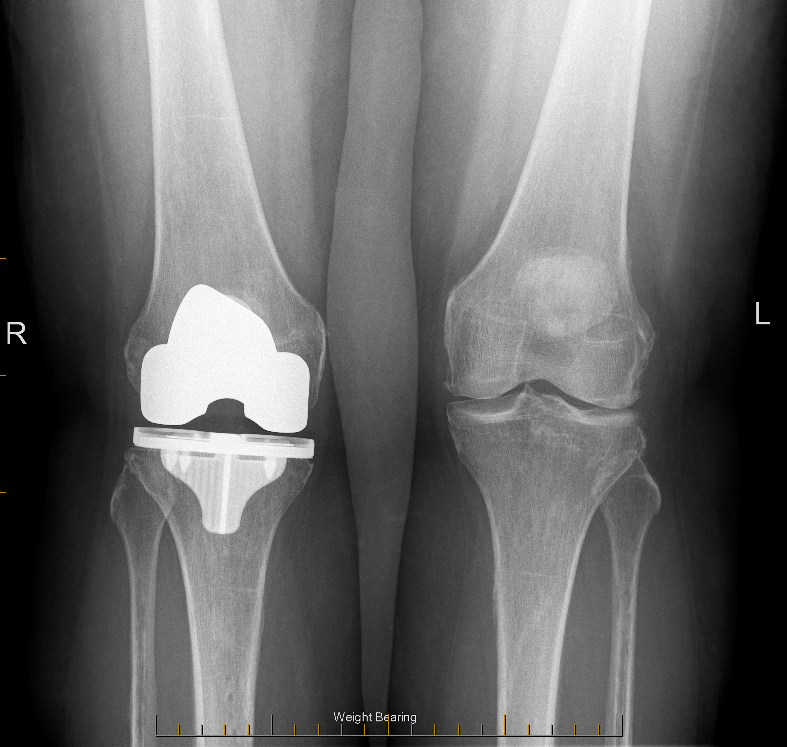
The surgeon removes the damaged parts of the knee joint, including the worn-out cartilage and bone. These are replaced with an artificial joint made of metal and polyethylene (a plastic material). The procedure is typically performed under a spinal anaesthesia that makes the lower half of your body numb, and typically takes under 90 minutes to complete.
For a total knee replacement, the entire knee joint is replaced with a new surface, whereas in a partial knee replacement, only the damaged area of the joint is removed and replaced with a prosthesis. Both can be done as robotic-assisted procedures (see below). The goal is to reduce pain, improve knee function, and help you return to more normal activities with less discomfort.
What to expect after surgery
Immediately following your knee replacement surgery, you can expect some discomfort and swelling, which is normal. Pain management will be provided through medications, and you will begin exercises and physiotherapy immediately after surgery to regain strength and mobility.
Here’s what you can expect in the first few days:
- Pain is typically managed through prescribed medications, including pain relievers and ice in the first days
- You will begin to move your knee soon after surgery under the guidance of physical therapists – this includes exercises to improve movement and strength
- It’s common to experience swelling around the knee, which may be treated with ice packs and elevation and can be present for 12 months or longer
Read the full rehabilitiation protocol below.
How long will you be in hospital?
Most patients stay in the hospital for one to three nights following knee replacement surgery, depending on their recovery progress and overall health. You will be monitored for signs of infection, blood clots, or other complications. Once you’re stable and able to move around with the assistance of crutches or a walker, you’ll be ready to discharge.
The recovery process after a knee replacement can vary from person to person:
- Within the first one to two weeks, you may need to use crutches or a walker – you will also begin a rehabilitation program that includes physiotherapy
- Many people feel a significant improvement within two months, with reduced pain and the knee functioning much better than before the surgery
- Full recovery can take six to twelve months as strength, flexibility, and function continue to improve
When can I drive after my surgery?
Generally speaking, most patients are driving again at 6 weeks after knee replacement surgery, and some do so earlier than this.
When you are able to drive depends on the following factors:
- Left or right sided surgery
- Automatic or manual car
- Medications being taken
- How quickly you recover from your surgery
For example, left sided surgery for an automatic vehicle driver may mean being able to drive much sooner than those with right sided leg surgery or those driving a manual vehicle. If you are still taking strong medications that can cause drowsiness such as morphine-derived or related pain killers (such as Palexia, Oxycontin, Endone, Tapentadol, Oxycodone, Tramal or Tramadol) it may also not be safe to drive.
There is no formal letter required from doctors for clearance to drive, and licencing authorities do not specify driving instructions after surgery. It is something discussed at your follow up visit and also somewhat self assessed as per below.
When you can walk comfortably or even hop on the operated leg then you are likely to be in a position to apply the brakes in an emergency without delay. It is recommended that you do this (apply the brakes suddenly) in a stationary, parked and turned-off vehicle when you feel that you are ready to drive again. If pain or stiffness limits your ability to break in an emergency, it may not yet be safe to drive. Feel free to talk to Dr Lambers or your GP about this if you have any concerns.
The arthroplasty society of Australia also has provided a statement which can be read below:
Possible risks
Knee replacement surgery, while highly effective, carries some risks:
- Infection is a primary concern, ranging from superficial wound infections, treatable with antibiotics, to rare deep infections affecting the prosthesis, which may require further surgery
- Blood clots, including deep vein thrombosis (DVT) or pulmonary embolism (PE), are another potential risk and can be life-threatening. These are mitigated through preventative measures like early mobilisation and blood-thinning medications.
- Rare complications include implant loosening, nerve injury, or impaired function, which may resolve over time or require intervention.
How long does a knee replacement last?
More than 90% of knee replacements last at least ten years. In many cases, a knee replacement can last 20 years or more. However, younger patients are more likely to need revision surgery at some point in their lifetime. See the graph below to see the chances of a second knee operation for your age and sex provided by the New Zealand Joint Replacement Registry. It is important to note that the majority of patients, at any age, will not have a second knee replacement.
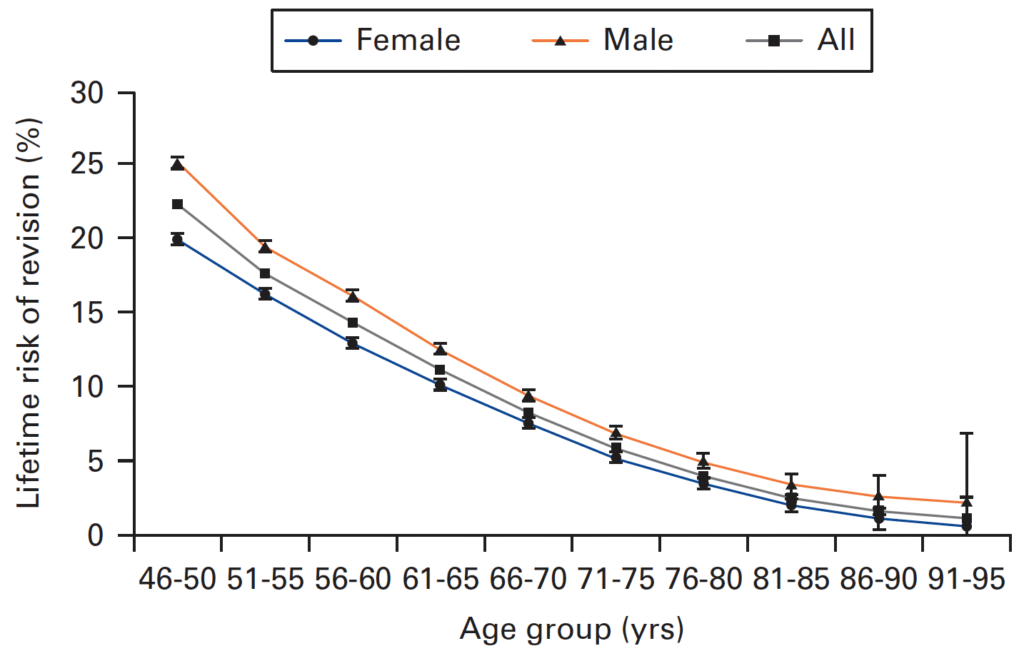
Source: Stone B, Nugent M, Young SW, Frampton C, Hooper GJ. The lifetime risk of revision following total knee arthroplasty : a New Zealand Joint Registry study. Bone Joint J. 2022 Feb;104-B(2):235-241. doi: 10.1302/0301-620X.104B2.BJJ-2021-0890.R1. PMID: 35094573.
Considering surgery
The decision to undergo surgery is a personal one, and it’s important not to rush it. Take time to fully understand your condition and treatment options, and consider whether joint replacement is the right choice for you. Your healthcare team, including Dr Lambers, can help guide you through the decision-making process and provide support every step of the way.
The choice to move forward with surgery is yours to make and there is usually no significant risk in delaying surgery. Take the time you need to consider whether knee replacement is the right step for you.

