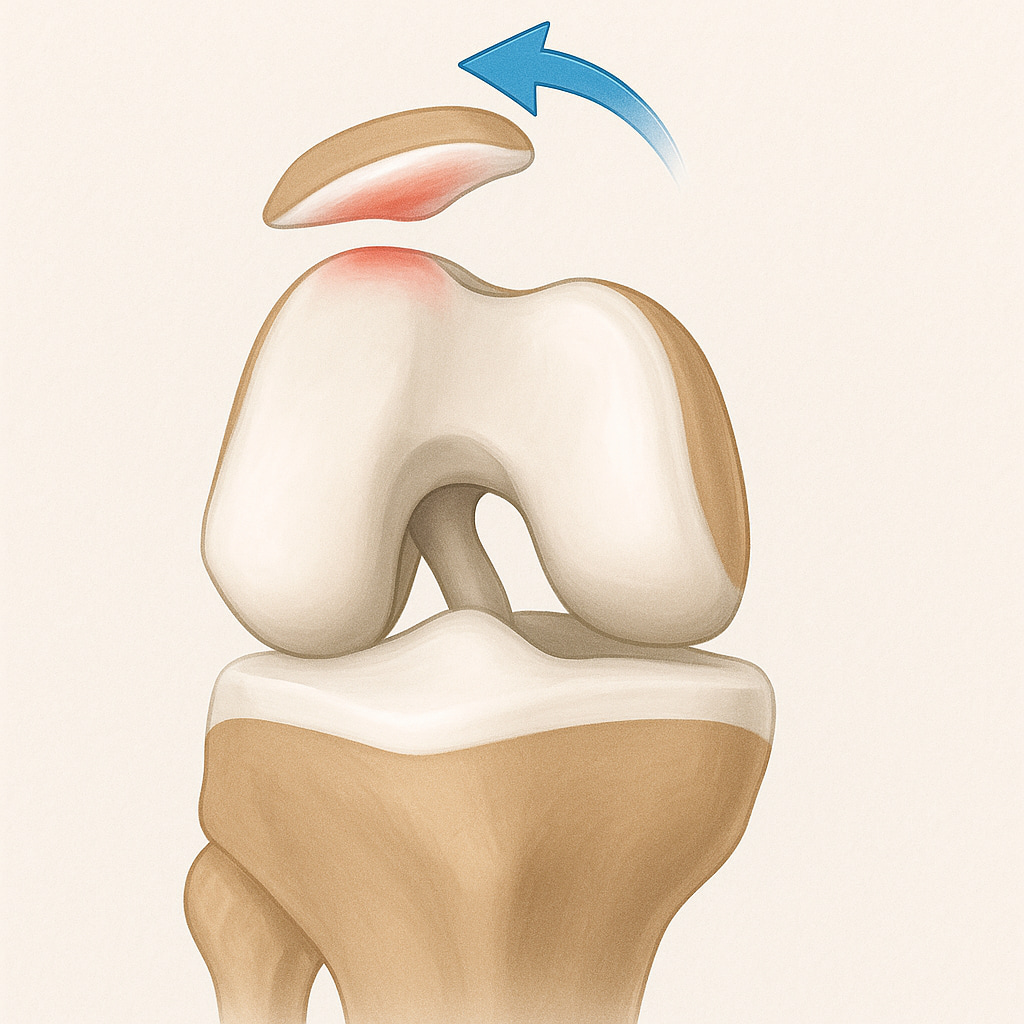
When surgery is recommended for conditions where the patella (kneecap) frequently dislocates or feels unstable, various options are available depending on the underlying cause of the instability. The aim of surgery is to restore stability and prevent further damage. Read more about kneecap instability below:
Indications for surgery
Surgery is considered for those who experience recurrent kneecap dislocations, persistent instability, or significant pain that does not improve with non-surgical treatments. In almost all patients that have a knee cap dislocation, physiotherapy without surgery is all that is required. Specific conditions that may necessitate surgery include:
- Multiple kneecap dislocations
- Damage to the stabilising ligaments
- Structural abnormalities, such as a high-riding kneecap (patella alta) or abnormal thigh or shin bone alignment
- Failure of physiotherapy or other non-surgical interventions to alleviate symptoms
What the surgery involves
The type of surgery depends on the root cause of the instability. Common procedures include:
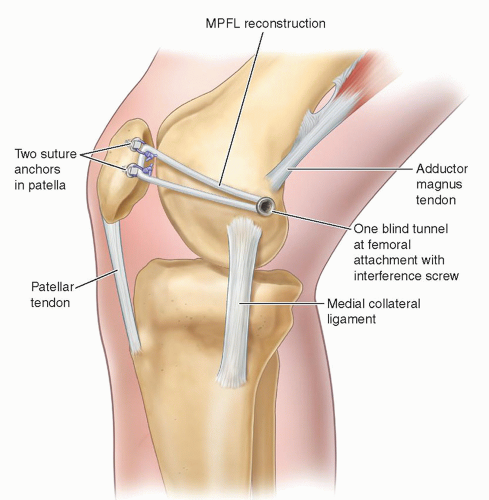
Medial Patellofemoral Ligament (MPFL) Reconstruction
This procedure replaces the damaged ligament that helps keep the kneecap in place. A small section of the hamstring tendon is used to create a new ligament, which is anchored to the thigh bone and kneecap. Read about the rehabilitation after surgery below:
Tibial Tubercle Transfer
This involves repositioning the attachment point of the patellar tendon below the kneecap to improve alignment and prevent dislocations. The tendon, along with a small piece of attached bone, is moved to a better position and secured with screws. Read about the recovery after this procedure below:

Arthroscopic Surgery
Sometimes performed alongside other procedures, arthroscopy involves small incisions and introduction of a small camera into the knee joint to repair soft tissue damage, assess knee cap position or treat other problems inside the joint.
Trochleoplasty
If the groove in the femur that guides the kneecap is too shallow (trochlear dysplasia), this procedure deepens the groove to improve patellar tracking. Dr Lambers does not provide this treatment but is happy to refer you onto another surgeon who does, if it is appropriate.
Distal Femoral Osteotomy
This procedure realigns the thigh bone to improve knee mechanics in cases where its abnormal rotation or angulation contributes to instability.
What to expect after surgery
Following surgery, the recovery process varies based on the type of procedure performed. Common postoperative experiences include:
- Pain and Swelling: These are typical but managed with prescribed medications
- Crutches and Brace: You may use crutches for 1-2 weeks and wear a brace to limit knee movement for up to 6 weeks, depending on the procedure
- Physical Therapy: Rehabilitation starts soon after surgery to restore mobility and strength gradually
How long will you need to spend in hospital?
Patients undergo knee cap stabilisation surgery as a day procedure. You’ll be discharged once you’ve recovered from the anaesthesia and received guidance on caring for your knee.
Usual recovery times
Recovery times depend on the procedure and individual healing rates:
- Weight-Bearing: You may begin bearing weight within 1-2 weeks, though activity restrictions may apply
- Sedentary Work: Typically resumed within a few weeks
- Sports and High-Impact Activities: It may take 4-6 months to safely resume, especially for procedures like MPFL reconstruction or trochleoplasty
Potential risks
- Joint stiffness may develop without proper post-operative rehabilitation
- Persistent pain and swelling in the form of complex regional pain syndrome
- Bleeding around the surgical site or inside the knee
- Although rare, joint infections may need antibiotics, knee lavage, or revision surgery
- Blood clots in the lungs or legs which can be life-threatening
- Poor healing or fractures during tibial tuberosity transfer may need revision surgery
- Recurrence of kneecap dislocations despite surgery
The decision to proceed with surgery
Dr Lambers recommends taking your time to weigh the benefits and potential risks of surgery. He is here to provide guidance and support to help you reach the right decision.

