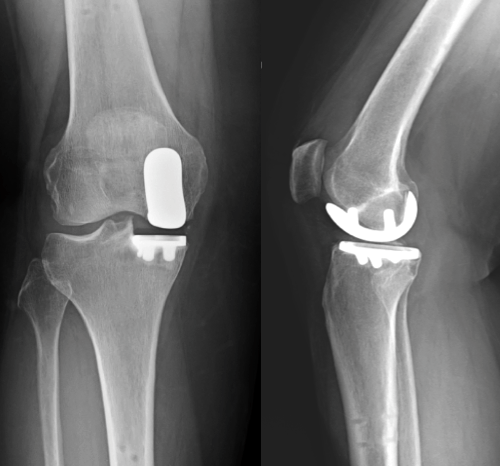
A partial knee replacement (which is also referred to as a unicompartmental knee replacement) is a surgical option for patients with arthritis confined to one knee compartment. There are three compartments in the knee, the medial (inner knee), lateral (outer knee) or patellofemoral (knee cap) compartments. Partial knee replacement is typically performed in the medial compartment but all three are possible.
It is recommended for individuals with:
- Medial compartment arthritis or, less commonly, arthritis in the lateral or patellofemoral compartments
- Otherwise healthy knee structures, such as intact ligaments and cartilage in the areas that won’t be replaced
- A stable knee joint with no significant deformities or ligament instability
- Those who wish to avoid a full replacement
- Normal or near-normal body weight
- Those with symptoms and x-ray findings that are localised to a single compartment
It may not be appropriate for those with inflammatory arthritis, obesity, severe knee stiffness, or significant angular deformities of the leg and Dr Lambers will discuss whether or not it would be suitable for you. Read more about knee arthritis in general below. The Australian Orthopaedic Association has information for patients to assist with how to manage with hip or knee arthritis whilst awaiting surgery, which can be accessed below.
What the surgery involves
Partial knee replacement focuses on resurfacing the damaged portion of the knee while preserving healthy bone, cartilage, and ligaments. The procedure typically involves an incision made over the front of the knee similar to that of a total knee replacement. The surgeon accesses the damaged compartment, leaving healthy structures untouched. Worn-out cartilage and bone are carefully removed from the targeted compartment, and trial components are used to ensure accurate sizing. Permanent metal and plastic implants are then secured to restore smooth joint movement. This is different to a total knee replacement where all three cartilage surfaces of the knee are replaced.
The wound is then closed with absorbable sutures, and an ice-compression bandage is applied to reduce swelling. Patients are encouraged to start moving their knee on the same day. Advanced techniques, including robotic assistance, may be used to precisely align and position the implant, enhancing the surgery’s outcomes. See the robotic joint replacement page below to learn more.
What to expect after surgery
- Significant reduction in arthritis-related pain in the treated compartment
- Better joint function and an ability to perform daily activities
- While the knee will feel more natural compared to a total knee replacement, minor clicking sensations or warmth in the knee during early recovery are normal and it is still likely to feel different or artificial
Read the full rehabilitation protocol here:
How long will you need to spend in hospital?
Most patients will need to stay in the hospital for 1 night though some go home the same day. Discharge typically occurs once the pain is manageable and patients can walk with assistance. Depending on their recovery progress and support system, some individuals may even return home the same day.
Walking and light activity are encouraged within the first few days. An outpatient physiotherapy program aids in restoring strength and mobility. Many patients can resume driving two weeks after surgery, provided they are no longer taking strong pain medications and most return to desk jobs within 2–3 weeks. Low-impact activities like golf and swimming are often resumed within 8–10 weeks, though full recovery can take 6-12 months.
Note: Swelling and some discomfort are normal during this period, but they should gradually decrease as healing progresses.
Potential risks
Some patients may still experience knee pain or limited mobility post-surgery. Rare complications include blood clots, infections at the surgical site or within the knee, and nerve or blood vessel damage. Prosthetic implants may loosen, wear out, or break. Scar tissue formation inside the knee can also restrict movement if a condition called arthrofibrosis occurs. It is common to have numbness around the scar after surgery.
While these risks are uncommon, following Dr Lambers’ advice and seeking medical attention if you notice wound problems or other concerning symptoms after the procedure is important.
How long does a partial knee replacement last?
More than 85% of partial knee replacements last at least ten years in Australian patients. In many cases, a partial knee replacement will last 20 years or more. However, younger patients as well as females are more likely to need revision surgery at some point in their lifetime. See the graph below to see the chances of a second knee operation for your age and sex provided by the New Zealand Joint Replacement Registry. It is important to note that the majority of patients, at any age, will not have a second knee replacement following a partial knee replacement and that is the aim of surgery. A partial knee replacement should not be considered as a temporary relief procedure.
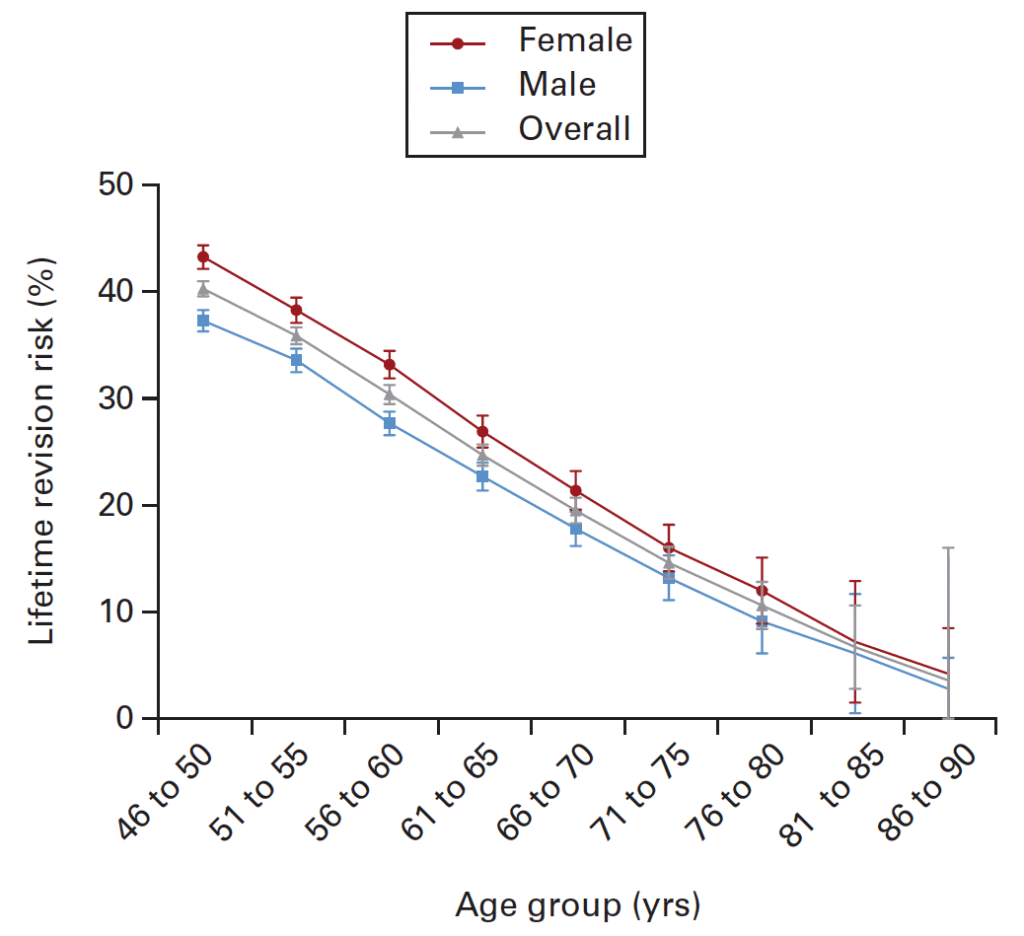
Source: Tay ML, Young SW, Frampton CM, Hooper GJ. The lifetime revision risk of unicompartmental knee arthroplasty. Bone Joint J. 2022 Jun;104-B(6):672-679. doi: 10.1302/0301-620X.104B6.BJJ-2021-1744.R1. PMID: 35638212.
Choosing surgery with Dr Lambers
Should your GP recommend surgery as a consideration, Dr Lambers will work with you to help you understand more about the procedure and if it is the right course of action.
This is a significant decision that should not be rushed. Take the time to explore all options, discuss your concerns with your GP and Dr Lambers, and carefully weigh the benefits and risks of a partial knee replacement.

