Is your hip pain making it difficult to perform simple daily activities?
Hip replacement surgery aims to reduce pain, improve mobility, and enhance quality of life. A hip replacement can provide long-term relief for those who have seen little improvements with medications, physical therapy, and lifestyle adjustments. Click below for more information about hip arthritis as a condition, to find a helpful decision-making guide about surgery and some advice for what to do while you wait for surgery if chosen.
What does hip replacement surgery involve?
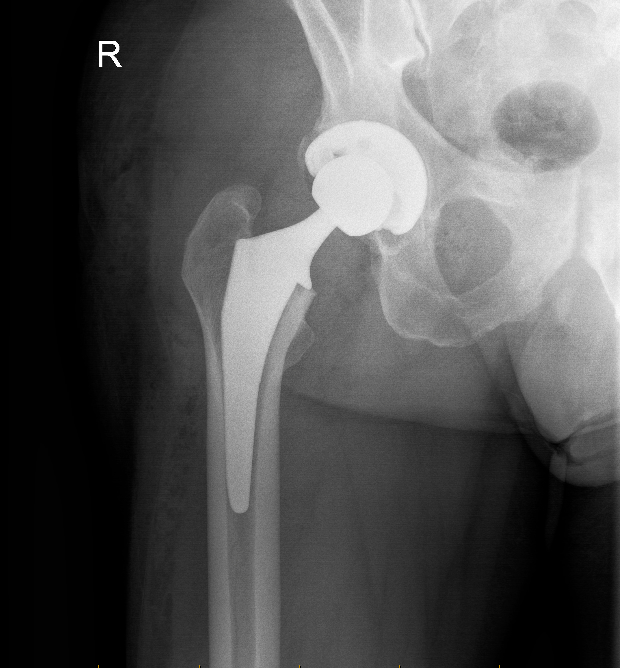
In this procedure, damaged parts of the hip joint are replaced with artificial components. The hip is a ball-and-socket joint where the femur (thigh bone) meets the pelvis. Over time, conditions like arthritis can cause the cartilage to wear away, leading to painful bone-on-bone contact. Read about arthritis of the hip here [Link to Condition Page].
The primary steps in the procedure are as follows:
- The head of the femur is removed, along with the damaged cartilage in the hip socket.
- The acetabulum (hip socket) is reshaped using a reaming tool to create space for the artificial cup.
- A new socket made of metal, plastic, or ceramic is implanted into the pelvis. The femoral head is replaced with a ball (made of metal or ceramic) attached to a stem placed inside the femur.
Dr Lambers uses robotic assistance during hip replacement surgery to ensure more precise placement of the components, which provides more reproducible component placement. If you would like to see what these implants look like in real life, ask Dr Lambers at your appointment and he can show you.
What to expect after hip replacement surgery
Recovery varies from person to person, but most patients will spend up to three days in the hospital after the surgery.
During this time, you’ll receive medications to manage pain, feeling sick and constipation. You’ll also start walking with assistance, typically the same day or the next after the surgery.
Rehabilitation
Physical therapy is a very important part of recovery. You’ll begin exercises to improve your range of motion and strengthen the muscles around the new joint. Occupational therapy may also be recommended to help you learn how to safely perform daily activities. See the full post-operative protocol following hip replacement below:
Returning to normal activities
Most patients can return to light activities—such as walking unaided—within 6 weeks of surgery. However, full recovery, which allows for low-impact sports like swimming or cycling, may take 3 to 6 months. To protect the new joint, high-impact activities, such as running or jumping, should be avoided in the first few weeks. Most people feel they are at maximum recovery by 12 months postoperatively.
Managing pain/discomfort
It’s normal to experience some discomfort and swelling in the weeks after surgery. Pain can be managed with medication up to a point, but there will be discomfort after surgery. You’ll also be given instructions on how to prevent complications, like blood clots, which will involve taking blood-thinning tablets or injections for six weeks after surgery.
When can I drive after my surgery?
Generally speaking, most patients are driving again at 6 weeks after hip replacement surgery, and some do so earlier than this.
When you are able to drive depends on the following factors:
- Left or right sided surgery
- Automatic or manual car
- Medications being taken
- How quickly you recover from your surgery
For example, left sided surgery for an automatic vehicle driver may mean being able to drive much sooner than those with right sided leg surgery or those driving a manual vehicle. If you are still taking strong medications that can cause drowsiness such as morphine-derived or related pain killers (such as Palexia, Oxycontin, Endone, Tapentadol, Oxycodone, Tramal or Tramadol) it may also not be safe to drive.
There is no formal letter required from doctors for clearance to drive, and licencing authorities do not specify driving instructions after surgery. It is something discussed at your follow up visit and also somewhat self assessed as per below.
When you can walk comfortably or even hop on the operated leg then you are likely to be in a position to apply the brakes in an emergency without delay. It is recommended that you do this (apply the brakes suddenly) in a stationary, parked and turned-off vehicle when you feel that you are ready to drive again. If pain or stiffness limits your ability to break in an emergency it may not yet be safe to drive. Feel free to talk to Dr Lambers or your GP about this if you have any concerns.
The Arthroplasty Society of Australia also has provided a statement which can be read below:
Potential risks and complications
Like any surgical procedure, hip replacement surgery carries some risks and is not to be taken lightly. However, it is considered an effective and worthwhile treatment for severe hip arthritis. Potential complications include:
- Infections that can occur at the incision site or deeper in the joint. In serious cases this can require further surgery to clean the joint or even removal of the new components.
- A deep vein thrombosis (DVT, leg clot) or Pulmonary Embolus (PE, a lung clot) can develop in your veins after surgery.
- The new ball can sometimes pop out of the socket (dislocate), especially in the first few months after surgery.
- In rare cases, surrounding nerves or blood vessels can be injured during the procedure. In worst-case scenarios this can leave you with permanent numbness or weakness in the lower leg.
- Some patients may feel that one leg is longer or shorter than the other after surgery. This most often relates to the feeling of the new joint rather than an actual difference in leg lengths.
Most complications are treatable, but following all post-operative instructions is important to minimise risks. The most important thing to prevent complications after surgery is to get moving early.
How long does a hip replacement last?
More than 90% of hip replacements last at least ten years. In many cases, a hip replacement can last 20 years or more. However, younger patients are more likely to need revision surgery at some point in their lifetime. See the graph below to see the chances of a second hip operation for your age and sex provided by the New Zealand Joint Replacement Registry. It is important to note that the majority of patients, at any age, will not have a second hip replacement.
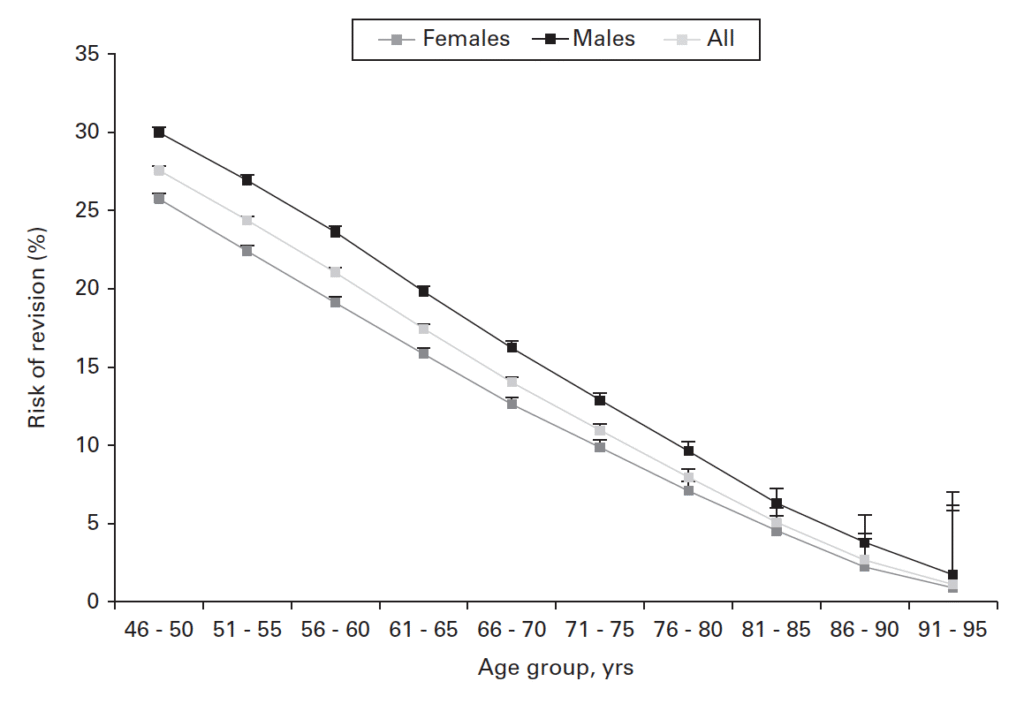
Source: Nugent M, Young SW, Frampton CM, Hooper GJ. The lifetime risk of revision following total hip arthroplasty. Bone Joint J. 2021 Mar;103-B(3):479-485. doi: 10.1302/0301-620X.103B3.BJJ-2020-0562.R2. PMID: 33641431.
Hip replacement surgery is a life-changing procedure for individuals with debilitating hip pain
This surgery can help you regain independence and get back to doing the activities you love by reducing pain, restoring mobility, and improving your quality of life.
If you’re suffering from hip arthritis and are considering hip replacement surgery, consult your GP for a referral to Dr Anton Lambers, who can assess your condition and determine if surgery could be beneficial for you.

