See Also:
Rehabilitation goals
- Protect the surgical repair and minimise swelling
- Restore ankle range of motion (ROM) within safe limits
- Re-establish muscle strength and endurance
- Improve proprioception and balance
- Progress to functional and sport-specific activities
Expected recovery time
| Milestone | Timeframe |
|---|---|
| Protected weight-bearing (crutches/boot) | 0–2 weeks |
| Transition to full weight-bearing | 2–6 weeks |
| Near-normal ankle ROM | 6–8 weeks |
| Progressive strengthening | 6–12 weeks |
| Proprioception and balance drills | 8–16 weeks |
| Return to low-impact activities | 12–16 weeks |
| Return to running/sport validation | 16–24 weeks |
Phase 1: Early Post-op (0–2 weeks)
Goals
- Protect the repair and control pain/swelling
- Begin gentle ROM within surgeon’s limits
- Maintain cardiovascular fitness (non-weight-bearing)
Instructions
- Immobilise in surgical boot or cast as directed
- Elevate the limb above heart level whenever resting
- Apply ice pack (wrapped cloth, approximately 0–5 °C) for 15–20 minutes, 3–4 times daily
- Manage pain with prescribed medications
Exercises
- Toe curls and ankle alphabet (in boot, gentle movement)
- Isometric ankle eversion/inversion against immobile resistance
- Hip and knee range-of-motion exercises (seated or supine)
Phase 2: Intermediate Mobilisation (2–6 weeks)
Goals
- Progress to full weight-bearing in boot or shoe
- Increase ankle ROM toward neutral dorsiflexion and plantarflexion
- Begin basic muscle activation
Instructions
- Gradually reduce crutch use, advancing to full weight-bearing as tolerated
- Remove boot for ROM exercises only, then re-apply
- Continue ice if swelling increases after activity
Exercises
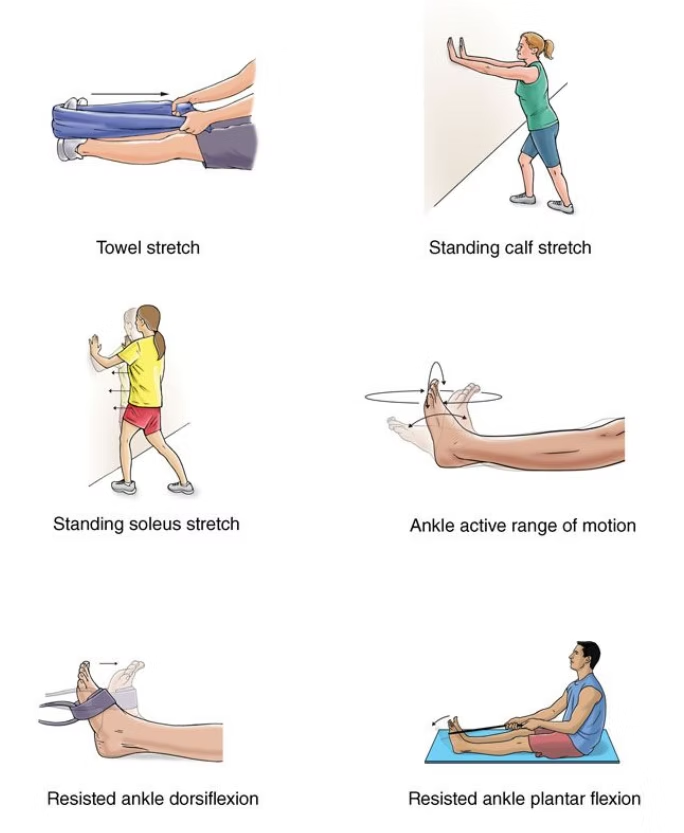
- Active-assisted dorsiflexion/plantarflexion and inversion/eversion
- Seated heel slides and towel stretches (hold 20–30 seconds)
- Standing weight shifts side to side and front to back (support as needed)
Phase 3: Strengthening and Proprioception (6–12 weeks)
Goals
- Achieve full, pain-free ROM
- Develop ankle and lower-limb strength
- Improve balance on stable surfaces
Instructions
- Transition into supportive athletic shoe with medial arch support
- Begin low-load functional activities (e.g. mini-squats)
- Incorporate proprioceptive training daily
Exercises
- Theraband resisted dorsiflexion, plantarflexion, inversion, eversion (3×15 reps)
- Calf raises (double-leg progressing to single-leg)
- Single-leg stance on firm surface (progress to foam pad)
- Step-ups and lateral step-downs
Phase 4: Advanced Functional Training (12–24 weeks)
Goals
- Restore dynamic stability and agility
- Reintegrate into sport-specific movements
- Ensure confidence in ankle during unpredictable tasks
Instructions
- Progress plyometric and cutting drills gradually
- Monitor for swelling and discomfort—ice as needed
- Coordinate with coach or therapist for return-to-sport criteria
Exercises
- Single-leg hop-to-stabilise in multiple directions
- Agility ladder drills (side-steps, carioca)
- Jog-run progression on even ground, then variable surfaces
- Sport-specific cutting, pivoting and jumping drills
When to contact your surgeon
- Increasing redness, warmth or drainage from incision
- Uncontrolled pain despite medications
- Numbness, tingling or loss of movement in foot/toes
- Sudden increase in swelling that does not improve with elevation
- Fever above 38 °C
Disclaimer
This is a general guideline. Your physiotherapist or Dr Lambers may adjust the protocol based on your specific condition and progress.
