See Also:
Rehabilitation Goals
- Ensure proper bone healing and fusion
- Control pain and swelling
- Protect the surgical site
- Restore strength and function to the surrounding joints and muscles
- Enable a return to walking and daily activities with assistive devices as needed
Expected Recovery Time
| Milestone | Timeframe |
|---|---|
| Non-weight bearing period | 0–6 weeks |
| Partial weight bearing | 6–10 weeks |
| Full weight bearing | 10–12+ weeks |
| Return to basic daily activities | 12–16 weeks |
| Return to low-impact work/activities | 4–6 months |
| Full recovery and function | 6–12 months |
Phase 1: Early Post-op (0–2 weeks)
Goals
- Protect the surgical site
- Minimize pain and swelling
- Begin gentle mobility for surrounding joints
Instructions
- Keep the leg elevated above heart level for most of the day
- Keep the cast or splint dry and intact
- Use crutches or a walker – non-weight bearing on the affected leg
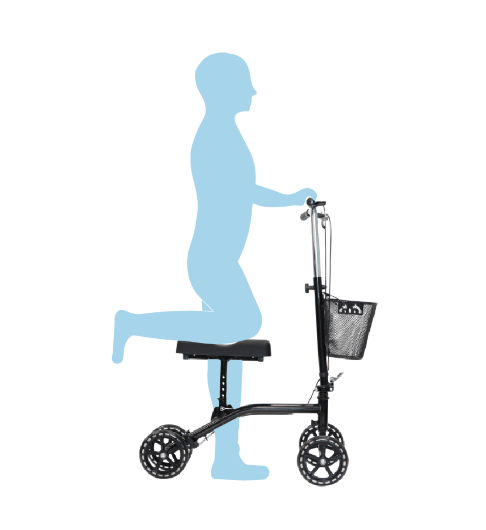
- Consider a kneelie scooter (pictured below)
- Ice the area (above the cast) for 15–20 minutes several times a day
Exercises
- Toe wiggling to promote circulation
- Isometric quad and glute contractions
- Gentle knee and hip range of motion (e.g., seated knee extensions)
Phase 2: Protected Healing (2–6 weeks)
Goals
- Continue protection of the fusion site
- Gradually increase mobility of the knee and hip
- Prevent muscle atrophy
Instructions
- Follow up for wound check and possible cast change or transition to a boot
- Remain non-weight bearing
- Continue use of crutches or walker
- Monitor for signs of infection (redness, increased pain, fever >38°C)
Exercises
- Continue toe, knee, and hip mobility
- Straight leg raises
- Seated ankle alphabet with the non-operated leg
Phase 3: Transition to Weight Bearing (6–10 weeks)
Goals
- Gradually introduce weight bearing as directed by the surgeon
- Begin gentle strengthening of the lower limb
- Maintain mobility of adjacent joints
Instructions
- Begin partial weight bearing as advised (often with a boot)
- Gradually reduce use of crutches/walker under guidance
- Attend physical therapy sessions if prescribed
Exercises
- Standing hip abduction and extension (with support)
- Gentle seated calf stretches
- Begin core and upper body conditioning
Phase 4: Functional Strengthening (10–16 weeks)
Goals
- Progress to full weight bearing
- Improve strength and endurance
- Focus on balance and gait training
Instructions
- Transition out of the boot to supportive footwear if cleared
- Continue physiotherapy to restore functional movement
- Avoid high-impact activities
Exercises
- Standing heel raises (bilateral to unilateral as tolerated)
- Balance exercises (e.g., single-leg stance with support)
- Low-resistance cycling or pool walking if approved
Phase 5: Return to Activity (4–12 months)
Goals
- Regain full function for daily and low-impact recreational activities
- Maximize joint and soft tissue mobility
- Build endurance and prevent compensatory patterns
Instructions
- Continue progressive loading and activity
- Use orthotics or ankle-foot orthosis if recommended
- Discuss return to work/sports with the surgeon
Exercises
- Full lower-limb strengthening (e.g., squats, step-ups)
- Proprioceptive drills (e.g., wobble board)
- Walking on varied surfaces, stair climbing
When to Contact Your Surgeon
- Increased redness, swelling, or warmth around the surgical site
- Fever above 38°C
- Persistent or worsening pain not controlled by medication
- Numbness or tingling in the foot
- Wound drainage or foul odor from the cast
- Difficulty or inability to bear weight when instructed to
Disclaimer
This is a general guideline. Your physiotherapist or Dr Lambers may adjust the protocol based on your specific condition and progress.
