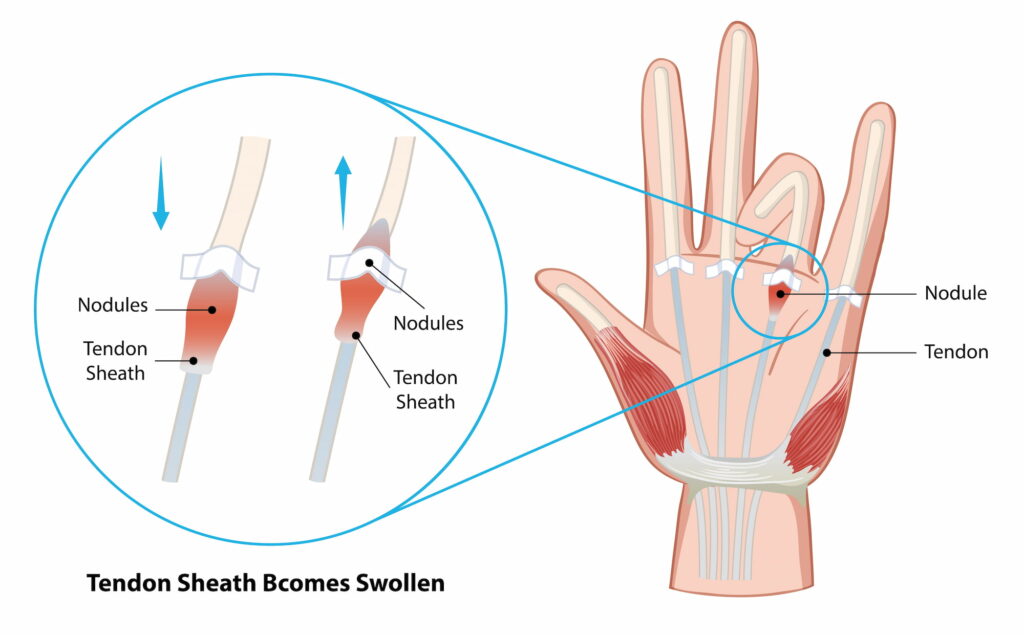
Trigger finger is characterised by difficulty in the smooth movement of a tendon within its sheath, often due to swelling or the formation of a small lump (nodule) on the tendon. This causes the finger to catch or lock in place, resulting in discomfort and restricted mobility.
What causes Trigger Finger?
Trigger Finger is the result of the tendon controlling the affected finger becoming irritated and swollen, making it difficult to glide smoothly through its protective sheath. In a significant number of cases, the exact cause of Trigger Finger is not clear, but irritation from overuse or systemic health issues plays a significant role. Common causes and risk factors include:
- Repeated motion or forceful gripping can irritate the tendon and cause swelling in the sheath
- A lump of tissue called a nodule, may form on the tendon, further restricting its movement
- People with conditions such as diabetes, low thyroid function, or rheumatoid arthritis are more likely to develop Trigger Finger due to changes in tendon health and inflammation
- The condition is most commonly seen in women over the age of 50
What symptoms would I notice?
The condition often affects more than one finger, and both hands may be involved. Symptoms tend to worsen in the morning or after periods of repetitive use.
- Finger stiffness noticeable in the morning or after periods of inactivity
- Popping or clicking as the tendon moves from a bent to a straight position
- A small bump may form in the palm at the base of the affected finger, often due to the swelling of the tendon sheath or the formation of a nodule
- The finger may lock in a bent position, and it may suddenly snap straight with discomfort or require manual manipulation to straighten
How is Trigger Finger diagnosed?
Diagnosis of Trigger Finger typically involves a combination of clinical evaluation and imaging tests. Your GP will begin by examining your hand for signs of stiffness, swelling, and any tenderness in the palm or fingers. They will also feel for a nodule or bump in the tendon sheath and test for triggering by asking you to move the affected finger.
X-rays may be ordered to rule out other conditions, and an Ultrasound is usually sufficient for diagnosis. CT or MRI scans are rarely required. If Trigger Finger is suspected, your GP may also refer you to a specialist like Dr Lambers for further evaluation or to discuss surgical treatment options.
Treatment options
Non-operative treatments
- Wearing a splint at night can help keep the affected finger in a neutral position, allowing the tendon to rest and reduce inflammation.
- Anti-inflammatory medications to reduce swelling and pain in the affected area
- Injecting cortisone into the tendon sheath can significantly reduce inflammation and help the tendon glide more freely (studies show that cortisone injections provide relief in up to 69% of cases and can prevent recurrence for three years or more)
- Physiotherapy and specific exercises can help improve tendon movement and reduce symptoms
Operative treatments
- Open Surgery
A small incision is made in the palm to release the tendon sheath and reduce the pressure on the tendon. This procedure is safe and highly effective, with a low risk of recurrence. It is performed as a day procedure.
- Percutaneous Needle Release
A less invasive approach where a needle is inserted to release the constricted tendon sheath, allowing the tendon to move freely. Whilst this has a smaller entry point, due to higher chances of the condition coming back Dr Lambers does not perform this procedure.
Read more about trigger finger surgery, and how it is safely performed with the patient awake under local anaesthetic (WALANT surgery) below:
Managing Trigger Finger with surgery
If non-operative methods have not provided sufficient relief, Dr Lambers will find the right procedure for your needs, along with guidelines for rehabilitation and recovery. The majority of patients experience significant improvement in their symptoms post-surgery, allowing them to return to normal activities without the limitations caused by their Trigger Finger.

