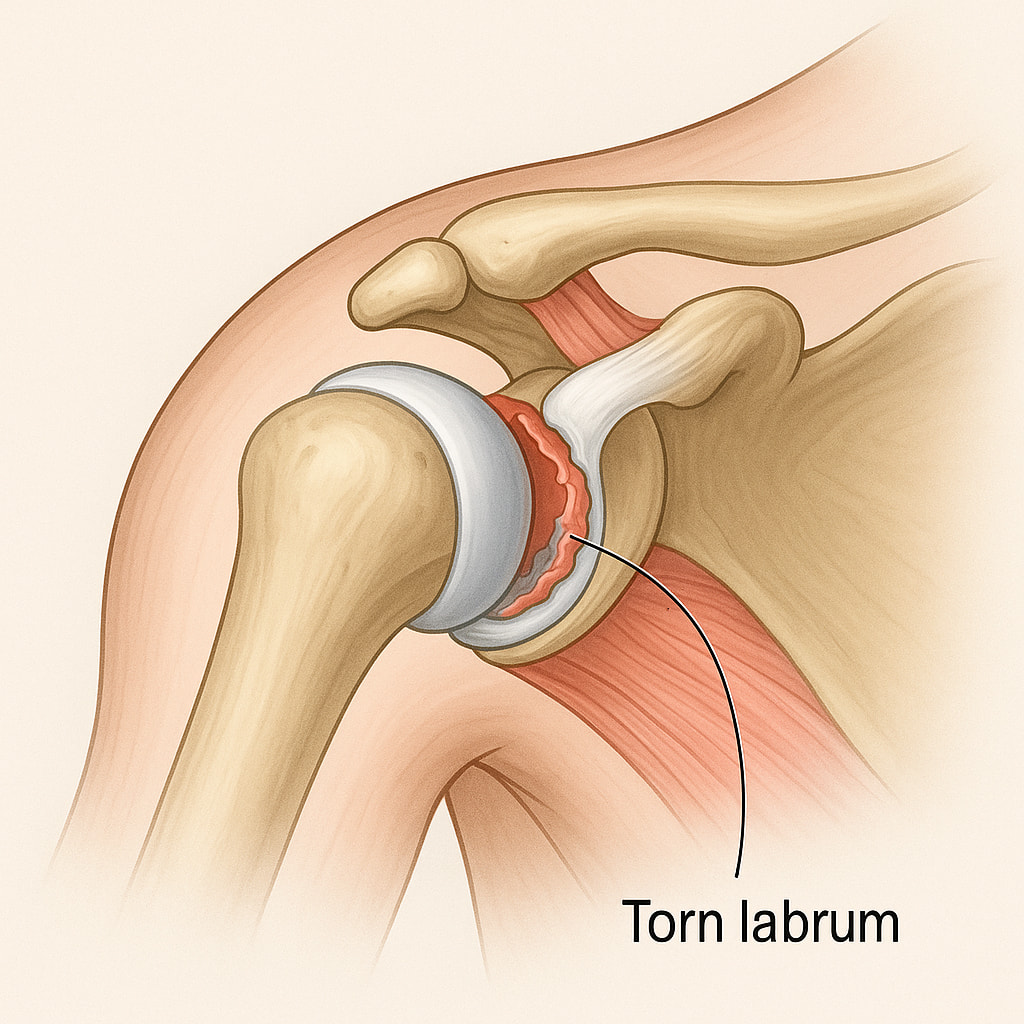
Unlike other joints, the shoulder’s wide range of motion makes it more susceptible to instability, especially if the supporting ligaments, capsule, or labrum (a ring of cartilage around the socket) become weakened, stretched, or damaged.
This condition can be a result of traumatic injury, repetitive use, or sometimes due to genetic factors that cause naturally looser ligaments.
What causes shoulder instability?
- A sudden impact, such as a fall or sports-related injury, can cause a shoulder dislocation or subluxation, leading to instability.
- Repeated overhead movements, like those in sports such as swimming, baseball, or tennis, can wear down the shoulder’s supporting structures.
- Some individuals have naturally loose ligaments, making them more prone to shoulder instability even without a significant injury.
- A prior shoulder dislocation often stretches or tears the ligaments and labrum, making the shoulder more likely to dislocate again.
What is happening inside my joint?
- Bankart Lesion: A labral injury, where the ring of cartilage that surrounds the socket is torn away from the bone, is known as a Bankart lesion. This normally acts to deepen the socket to increase stability.
- Bone Loss: Over time if many dislocations occur the bone of the socket can also wear away, or a severe injury can break bone away in the first episode. When this happens as part of the first injury it is referred to as a “Bony Bankart Lesion”.
- Hill-Sachs Lesion (HSL): If the head gets stuck onto the rim of the socket you can also create a hole or trench in the head that makes further dislocations more likely. This divot of bone is called a Hill-Sachs Lesion (HSL).
What symptoms would I notice?
- A sensation that the shoulder is “giving out” or slipping out of place.
- Recurrent shoulder dislocations or subluxations (abnormal movement without dislocation) with certain movements or activities.
- Pain, especially after a dislocation or certain arm movements, is common and can range from mild to intense.
- You may notice a reduced ability to move your arm fully, along with possible swelling and bruising.
How is shoulder instability diagnosed?
Your GP will ask you questions and perform an examination to assess the shoulder’s range of motion, strength, and points of tenderness. Specific tests are often used to assess joint laxity and X-rays will be used to rule out fractures or other bone-related issues.
An MRI scan with injected dye may be recommended to visualise the shoulder’s soft tissues, such as the labrum and ligaments, and check for tears or other injuries. In cases with suspected bone loss, a CT scan may be used to provide detailed images of the shoulder’s bony structures.
Treatment options
The treatment will depend on the severity of the instability and the frequency of dislocations. Non-surgical treatments are often preferred, especially for first-time dislocations in patients over 30. As you get older, your joint structures become more stiff lowering your chance of another dislocation.
Non-operative treatments
- Exercises to strengthen the muscles around the shoulder, in particular, the rotator cuff and scapular stabilisers, help improve shoulder stability and support.
- Paracetamol and Ibuprofen to help reduce pain and inflammation.
- Avoiding activities that strain the shoulder can help prevent further dislocations.
- A sling may be used after the initial injury briefly to limit movement and allow healing, however this should be followed by sling removal and shoulder exercises to avoid stiffness.
Operative Treatments
Surgery may be considered if:
- There is recurrent shoulder instability that does not improve with non-surgical methods.
- The individual is a competitive athlete (especially those aged 15–25) with a single dislocation and wants to minimise the risk of repeated instability episodes.
Operative treatment options include:
- Bankart Repair: arthroscopic “keyhole” surgery, a minimally invasive option that uses a small camera (arthroscope) to repair torn or stretched ligaments and labrum, reducing shoulder laxity.
- Remplissage: if there is a Hill-Sachs Lesion this may be filled in using suture anchors as an additional procedure to the Bankart Repair. This pulls the tendons and joint capsule into the bone defect to decrease the likelihood of further dislocation after surgery.
- Latarjet Procedure: open surgery for cases with bone loss of the socket. Dr Lambers would move a piece of bone with muscles attached to the front of the shoulder joint as a block to dislocation of the head, helping to stabilise the shoulder. This is performed for all patients with significant bone loss where keyhole surgery is likely to still allow repeat dislocations.
See below for more detailed information about surgery options for shoulder instability:
Shoulder instability surgery with Dr Lambers
Dr Lambers’ surgical options focus on restoring shoulder function and preventing future dislocations. Once non-operative treatments have been exhausted, your GP will refer you to Dr Lambers to discuss paths to return to your daily activities with confidence.

