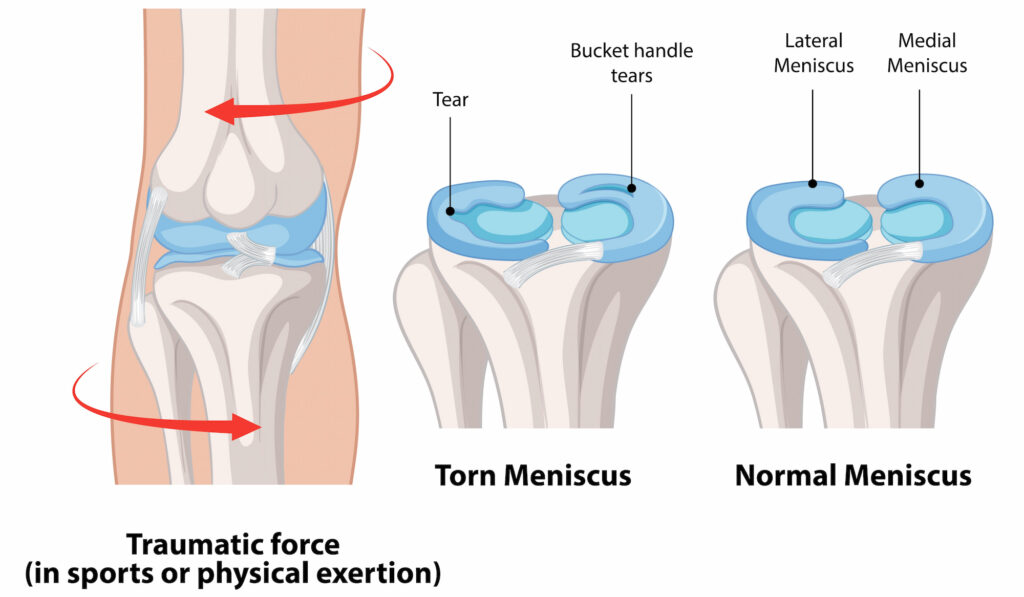
The meniscus is a crucial, rubbery knee structure that acts as a shock absorber and contributes to knee stability. Each knee has two menisci – one on the inner side called the medial meniscus, and one on the outer side called the lateral meniscus. They protect cartilage from excessive wear and tear.
Meniscal tears can be caused by sudden trauma or gradual degeneration. Traumatic tears often affect younger individuals, usually from a sports injury or twisting motion, and these patients have cartilage that is smooth and healthy. In contrast, degenerative tears commonly impact those over 40 as a part of the natural aging process and wear on the knee joint. Degenerative tears commonly exist alongside arthritis of the cartilage and are thought to be part of the same disease process. The two types of tears are different and are therefore treated differently.
What causes a meniscal tear?
Meniscal tears are classified into two main types: traumatic and degenerative. Traumatic tears, common in athletes and younger people, often result from twisting, turning, or pivoting the knee.
Degenerative tears occur gradually with age as the meniscus tissue weakens and becomes more susceptible to wear and tear. Over time, arthritis can also contribute to degenerative meniscal damage as roughened cartilage and bone rub against the meniscus.
What symptoms would I notice?
Common meniscal tear symptoms can include pain, swelling, and tenderness around the knee joint. You may experience sensations of clicking, catching, or even a “locking” feeling where the knee seems to get stuck. You may also notice some instability, feeling like your knee is “giving way.”
If you’re experiencing persistent knee pain, swelling, or mechanical symptoms like catching and locking, it’s important to consult your GP. If your knee is stuck locked in the one position and cannot be bent at all, you should consider attending your nearest emergency department or your GP as you may need more urgent treatment.
How is a meniscal tear diagnosed?
Diagnosing a meniscal tear with your GP typically involves a combination of answering some questions, a physical exam and imaging. Your GP will first review your symptoms and examine your knee. If the x-ray is normal, an MRI is often recommended to visualise the meniscus properly, as it provides a clear image of soft tissue structures, including the menisci and surrounding cartilage, which cannot be seen on x-ray alone.
Treatment for meniscal tears
Many meniscal injuries, particularly degenerative tears, are managed with conservative measures. Surgery is only recommended in certain cases, such as large tears that disrupt knee function in patients without arthritis. Your doctor will recommend the best course based on your specific condition:
Non-operative treatments
Non-surgical treatment is often effective for managing meniscal tears, especially if symptoms are mild. Resting the knee, modifying your activities, applying ice, and using anti-inflammatory medications can help reduce pain and swelling. Home based exercise programs guided by a physiotherapist can help to strengthen the surrounding muscles and improve your symptoms.
Non-operative treatments are usually all that is needed in the majority of meniscal tears. This is particularly true for smaller tears that are still sitting in a good position in young patients who don’t have significant symptoms and almost all degenerative tears.
Operative treatments
For large traumatic tears or those causing significant symptoms, surgery may be necessary. Arthroscopic surgery is minimally invasive and a way to either trim or repair the damaged portion of the meniscus.
In younger, active patients, a meniscal repair is performed when the tear is considered reparable; otherwise, it is trimmed. In degenerative cases, keyhole surgery is unlikely to provide lasting relief, and if the associated arthritis is severe enough, knee replacement may be considered when appropriate.
Read more about meniscal surgery and the rehab protocols below:
Managing meniscal tears with Dr Lambers
In all cases, your first step should be visiting your GP, where you can be assessed, diagnosed and all non-surgical treatments will be explored. If surgery is to be considered, your GP will refer you to Dr Lambers to discuss the next steps.

