What is hip arthritis?
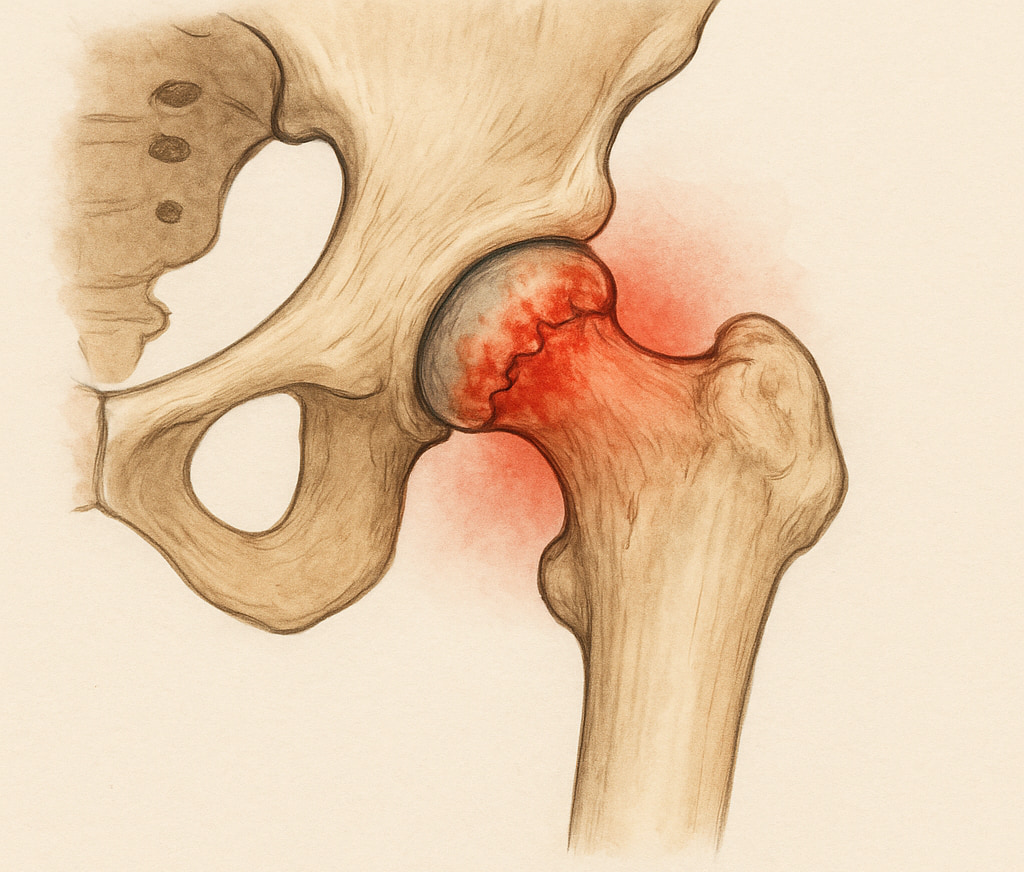
Hip arthritis affects the hip joint, one of the body’s largest and most important. The hip is a ball-and-socket joint, where the head of the thigh bone (femur) fits snugly into the pelvis socket (acetabulum). This joint is designed to provide smooth, pain-free movement, cushioned by a cartilage layer covering both the femur and the acetabulum (the socket).
In cases of hip arthritis, this cartilage gradually wears down, leading to painful friction between the worn cartilage or the exposed bones. Over time, the joint becomes stiff and painful, making everyday activities like walking, sitting, or bending increasingly difficult.
The most common type of hip arthritis is osteoarthritis, which results from the gradual wear and tear of the cartilage. Other forms include inflammatory arthritis (which encompasses conditions like ankylosing spondylitis, lupus, rheumatoid arthritis and gout) or post traumatic arthritis (that follows injury).
What causes hip arthritis?
Hip arthritis can arise from several factors, some of which are within our control, while others are not. Some primary causes include:
Previous injury
A significant injury to the hip, such as a fracture or dislocation, can lead to post-traumatic arthritis. This form of arthritis may develop years after the initial injury, as the joint’s natural alignment and cartilage may be permanently affected.
Genetics
If your parents or grandparents had hip arthritis, you may be more likely to develop it yourself. Genetics can influence the shape and stability of the hip joint and the strength of your cartilage, making you more susceptible to wear and tear.
Ageing
Our joints naturally undergo a certain degree of wear and tear as we age. The older you get, the more likely you are to develop osteoarthritis.
Obesity
Excess body weight adds stress to the hip joints. Over time, this can accelerate the wear and tear of the cartilage, leading to earlier onset of arthritis.
What symptoms would I notice?
Hip arthritis manifests in several ways, and the symptoms often depend on the severity of the condition. Many people can have arthritis without any symptoms as well. Common symptoms include:
Decreasing movement (stiffness)
You may find it increasingly difficult to move your hip joint, particularly after inactivity, such as waking up in the morning or sitting for long periods. Everyday tasks like putting on socks and shoes, getting out of a chair, or climbing stairs may become challenging.
Groin, outer hip, or buttock pain
Pain is a hallmark symptom of hip arthritis. You might feel a deep, aching pain in the groin area, but it can also spread to the outer hip, buttocks, or even down the thigh to the knee. This pain is often worse after activity or at the end of the day and can interfere with sleep.
Limping or difficulty walking
As the condition progresses, you may notice a limp due to the pain and stiffness in your hip. Walking, standing, and other weight-bearing activities may become increasingly painful.
How is hip arthritis diagnosed?
The diagnosis of hip arthritis is confirmed after seeing your GP, who will ask questions about your symptoms, examine your hip and confirm a worn-out hip joint via X-rays. X-rays can reveal the extent of cartilage loss, bone spurs (osteophytes), and other changes typical of arthritis. Usually, no further scans are required. In some cases, it may be necessary to rule out other causes of hip pain with MRI or CT scans.

Non-operative treatment
Treatment for hip arthritis typically starts with non-operative measures before considering surgical options.
Exercise and physical therapy
Regular, low-impact exercises can help maintain joint mobility and strengthen the muscles around the hip. An exercise program can also help manage symptoms and improve overall joint health. Stretching is also important, and it can preserve or even improve movement.
Weight management
Lowering weight can reduce stress on your hip joints, potentially slowing the progression of arthritis and often alleviating pain.
Activity modification
Altering your daily activities to avoid excessive hip stress can help manage arthritis symptoms. This might involve using walking aids, avoiding high-impact exercises, or taking frequent breaks during activities that require prolonged standing or walking.
Pain Management
Over-the-counter pain medications, such as paracetamol or anti-inflammatories, can help with pain and inflammation. Stronger medications, such as morphine-type medications, are not typically recommended for long-term conditions like arthritis. Corticosteroid injections may be used occasionally for flare-ups or as a test if the exact source of the pain is unclear.
Lifestyle changes
In addition to weight management, quitting smoking and maintaining a balanced diet may support joint health and slow the progression of arthritis. Supplements such as calcium, vitamin D, glucosamine and fish oil have not been proven in robust clinical trials to have any effect. Viscosupplementation injections such as Synvisc or Durolane have also not been shown to be consistently better than placebo injections (no medication) in major randomised trials, and these cannot reverse the changes of arthritis.
Operative treatment
Hip replacement surgery may be recommended when non-operative treatments no longer provide sufficient relief. In the right patient, hip replacement is a highly effective procedure for significantly reducing pain and restoring function in cases of advanced hip arthritis. An artificial joint that mimics the natural movement of a healthy hip replaces the damaged joint, allowing for a significant improvement in mobility and a reduction in pain. This can be performed with the assistance of advanced technology during the procedure, referred to as robotic surgery.
While surgery can be daunting, hip replacement has a high success rate and can improve your quality of life. Dr Lambers will discuss the procedure in detail, including the risks, benefits, and expected recovery process. You can read more about hip replacement, recovery after surgery and robotic surgery below.
The following two well-written resources are here to assist you with the decision making process around your treatment decision, as well as to provide you with advice with how to manage your hip arthritis while waiting for surgery if it is chosen.
Managing hip arthritis with Dr Lambers
Managing hip arthritis can be challenging, but many people can stay active and control their symptoms for a long time without surgery. If you’re dealing with hip pain or stiffness, your first step should be visiting your GP. They can assess your symptoms, examine you, and, if needed, arrange an X-ray to confirm whether it’s hip arthritis or another issue. If you’ve explored all the non-surgical treatments and your condition affects your quality of life, your GP may refer you to Dr Anton Lambers to discuss whether surgery could be the next step.

