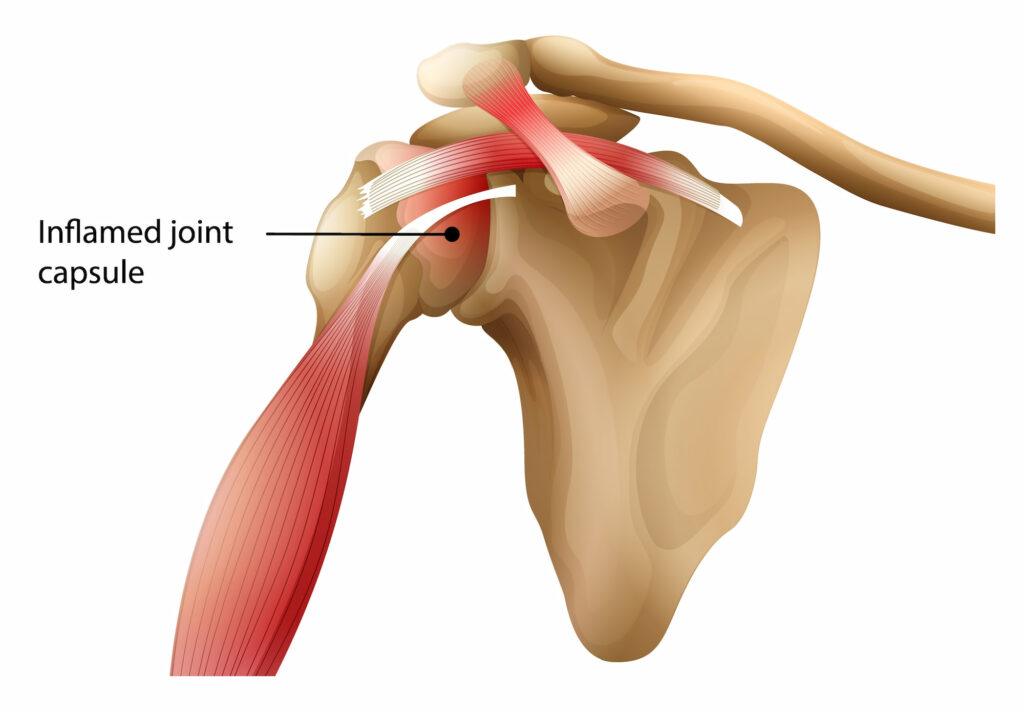
Frozen shoulder typically develops gradually, leading to a restricted range of motion as the shoulder capsule—the flexible tissue around the joint—thickens and tightens. This tightening reduces movement within the shoulder, leading to a “frozen” feeling.
Frozen shoulder is most common among individuals aged 40 to 60 and tends to affect more women than men. It is medically referred to as Adhesive Capsulitis.
What causes frozen shoulder?
The exact cause of frozen shoulder is not fully understood, but it often occurs following a period of immobility due to an injury, surgery, or underlying health conditions.
Certain groups of people are more at risk, including:
- Individuals with diabetes or thyroid disorders
- People with heart disease or Parkinson’s disease
- Those recovering from shoulder injuries or surgeries where movement was limited for an extended period
What symptoms would I notice?
Frozen shoulder progresses through three stages, each with distinctive symptoms:
- The Freezing Stage
This is the painful stage, where shoulder movement starts to become limited. Pain is present at rest and increases with shoulder movement. This stage can last from six weeks to nine months.
- The Frozen Stage
In this stage, the pain may diminish, but stiffness increases significantly, limiting shoulder movement even more. Simple activities like reaching overhead or behind the back become difficult. This stage can last four to six months.
- The Thawing Stage
The shoulder slowly begins to regain movement as the scar tissue gradually loosens. The pain subsides, and shoulder motion improves. This final phase can last six months to two years.
How is frozen shoulder diagnosed?
A GP will assess your shoulder’s range of motion and pain. An X-ray is typically conducted to rule out other shoulder issues like arthritis. In some cases, additional imaging, like an MRI, may be recommended to examine soft tissue involvement further.
Treatment options
Nearly all cases of frozen shoulder will resolve with non-operative methods aimed at reducing pain and restoring movement gradually. If non-operative treatments do not provide relief after several months, surgical options may be considered.
Non-operative treatments
- Physiotherapy exercises are essential for restoring shoulder mobility and function. Stretching and strengthening exercises help to ease stiffness and improve shoulder movement. It is important that these are performed gently in the painful stages and in combination with anti-inflammatory medications so that the condition is not aggravated.
- The Hydrodilatation procedure, which involves injecting a saline solution into the shoulder joint under ultrasound guidance to stretch the capsule, has not been shown to provide lasting benefit compared to steroid injection alone and therefore is not typically recommended.
- Anti-inflammatory medications and cortisone injections may be prescribed to manage pain and inflammation, especially during the initial “freezing” stage.
Operative treatments
- Arthroscopic Capsular Release
This minimally invasive “keyhole” surgery is performed to remove scar tissue and adhesions within the joint. Arthroscopic release can improve shoulder movement and provide pain relief, especially for individuals who have persistent symptoms despite other treatments. This is only considered after a full course of non-operative treatment has been attempted with your GP, which may take 9 months or longer to resolve.
- Manipulation Under Anaesthesia
During this procedure, the shoulder is gently manipulated while you are under anaesthesia, which helps break up scar tissue and increase range of motion. This can be performed as an isolated procedure or combined with arthroscopy so that it is performed in a controlled fashion after the tissues have been released surgically.
For cases requiring surgical intervention
Dr Lambers performs arthroscopic capsular release with manipulation. He will guide you through each step of the treatment process, from diagnosis and pre-operative preparation to post-surgical rehabilitation. Following surgery, a rehabilitation plan will be developed to help restore shoulder function and prevent future complications.

