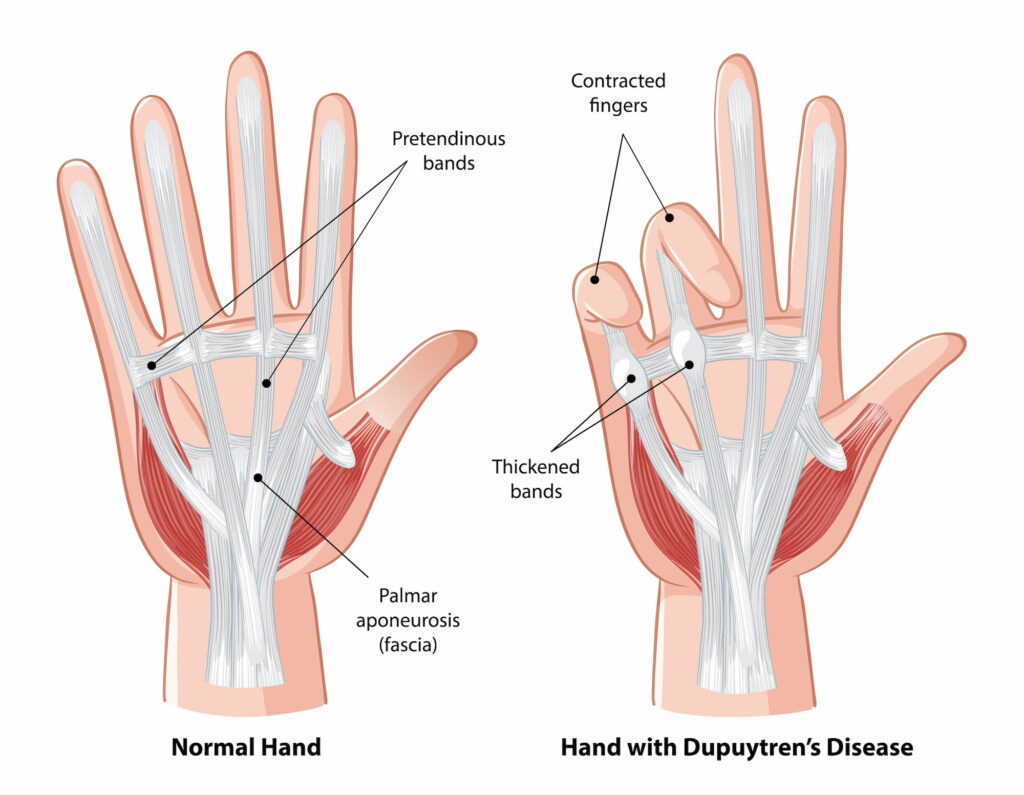
Dupuytren’s disease, also known as Dupuytren contracture, is a condition where abnormal scar tissue forms in the palm, gradually developing thick cords under the skin. Over time, these cords pull the fingers inward, causing them to bend towards the palm and restrict movement.
This typically affects the ring and little fingers, though it can involve other digits. While the condition doesn’t usually cause pain, it can significantly impair daily activities such as shaking hands, putting on gloves, or placing your hands in your pockets.
What causes Dupuytren’s Disease?
The exact cause of Dupuytren’s disease is unknown. However, certain risk factors can increase the likelihood of developing Dupuytren’s disease:
- It typically develops after the age of 50
- Men are more likely to develop it than women, and symptoms can be more severe in men
- Northern European descent is a known risk factor
- The condition often runs in families
- Diabetes, alcohol use, and smoking can increase the risk of Dupuytren’s disease
What symptoms would I notice?
In its early stages, Dupuytren’s disease may cause a small, firm lump in the palm, which can be painless or tender. As the condition progresses, this lump can extend into a cord-like structure that tightens and pulls the fingers towards the palm. Dupuytren’s disease often affects both hands and can progressively worsen if left untreated.
Symptoms often develop slowly over time and can include:
- Stiffness in the fingers that gradually worsens
- A hard lump or cord under the skin in the palm, which may be painful in some cases
- Difficulty straightening the fingers, especially the ring and little fingers
- The fingers bending towards the palm, which may interfere with daily tasks such as putting on gloves, using your hands for gripping, or shaking hands
- It sometimes also exists in the soles of the feet and in the penile tissue in males.
How is Dupuytren’s Disease diagnosed?
Diagnosis of Dupuytren’s disease generally involves a physical examination and a thorough medical history. Your GP will assess the condition’s progression, checking for the characteristic lumps and cords in the palm and fingers. In most cases, additional imaging such as X-rays or MRIs are not required for diagnosis. However, in some cases, imaging may be recommended to assess the severity or rule out other conditions that might mimic Dupuytren’s.
Treatment options
While there is no cure for Dupuytren’s disease, various treatments are available to relieve symptoms and slow its progression. The choice of treatment depends on the severity of the condition, the affected finger, and your overall health.
Read the below decision making guide from the NHS (UK) to help you in considering your treatment options with evidence to support the different options:
Non-operative treatments
- Wearing a splint can help in the early stages to keep the affected fingers in a more neutral position when the pull on the fingers is still flexible and the fingers can be straightened
- Hand therapy and stretching exercises to limit or slow down contractures
Operative treatments
If Dupuytren’s disease progresses to the point where it affects hand function or interferes with daily activities, surgery may be considered:
- Percutaneous Needle Fasciotomy
This is a room-based procedure where the cord is released using a needle. It offers a quick recovery time but has a high rate of recurrence (around 85% within five years).
- Xiaflex (Collagenase Injection)
This non-surgical treatment involves an injection of a special enzyme to break down the cord tissue, allowing for better movement. This product is no longer available in Australia.
- Fasciectomy
This is a more invasive surgery where the thickened tissue is removed. It’s typically recommended when other treatments have not been effective.
- Dermofasciectomy
In cases where Dupuytren’s disease is severe and the cord involves the skin, a dermofasciectomy (skin and cord removal) may be necessary. This procedure involves removing the skin and the underlying thickened tissue, followed by a skin graft.
- Amputation
In cases that present with severe contractures, an amputation may be the most appropriate procedure. Recovery is rapid and it removes the possibility of the condition recurring in that finger, which is common in severe cases if fasciectomy is performed. It is mainly considered in the little finger.
Read more about the surgical treatments and the expected recovery timeline below:
Managing the condition with surgery with Dr Lambers
If surgery is required to treat Dupuytren’s disease, Dr Lambers will assess and recommend the appropriate treatment. While there is a risk of recurrence, particularly after less invasive treatments like needle fasciotomy, Dr Lambers works closely with you to manage expectations and provide the necessary post-surgery care for optimal recovery.

