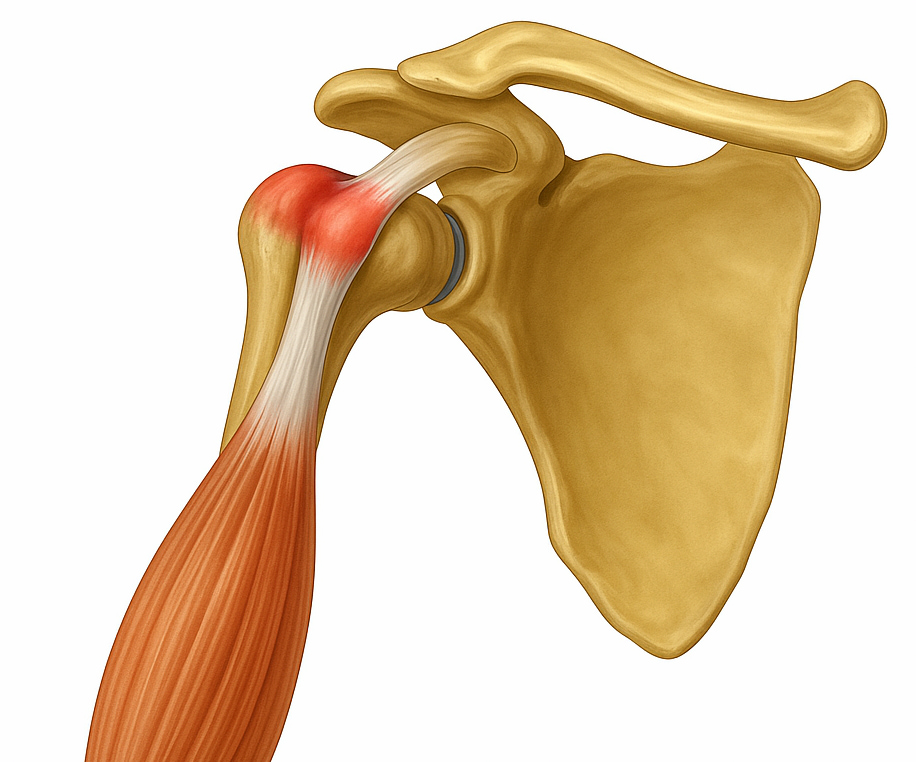
A biceps tendon tear happens when one of the tendons that attaches the biceps muscle to the shoulder or elbow is partially or completely torn. This tendon tear most commonly occurs in the shoulder and will affect the long head of the biceps tendon. The tear may sometimes impact other shoulder structures in the shoulder, like the rotator cuff. Despite the tear, many people can continue to use their arm with minimal discomfort or strength loss due to the two-point attachment of the biceps muscle.
This page discusses biceps tendon tears in the shoulder. Rupture of the biceps tendon in the elbow is an injury that requires prompt referral to your nearest emergency orthopaedic service in case surgery is required.
What causes a biceps tendon tear in the shoulder?
- A fall onto an outstretched arm or lifting something heavy may tear the tendon.
- A gradual wear down over time due to repetitive movements, especially in sports like swimming or tennis or jobs that involve heavy overhead lifting.
- Tendons weaken with age, making older individuals more at risk.
- Smoking and corticosteroid medications can weaken tendons and reduce muscle strength.
What symptoms would I notice?
- Pain at the front of the shoulder, possibly radiating down the front of the upper arm
- Tenderness in the shoulder, particularly in the deep front area
- Weakness in shoulder or elbow movements
- Cramping of the biceps muscle, especially with strenuous use
- A visible bulge in the upper arm (commonly known as the “Popeye” sign) due to the torn tendon
- Bruising on the upper arm, extending towards the elbow, after it was injured
- An audible “pop” may be heard at the time of the injury
How is a biceps tendon tear diagnosed?
Your GP will assess any physical deformities or muscle weakness, examining the shoulder and arm, looking for signs of a complete or partial tear. An ultrasound or MRI can commonly be used to confirm a biceps tendon tear. An MRI provides a clear view of soft tissue injuries, while X-rays help identify other shoulder issues.
Treatment options
For most individuals, non-operative treatments are effective, but surgical intervention may be recommended if symptoms persist.
Non-operative treatments
- Avoiding heavy lifting and repetitive shoulder movements can minimise pain.
- Ice packs on the shoulder can help reduce inflammation.
- Nonsteroidal anti-inflammatory medication such as ibuprofen or naproxen may relieve pain and reduce swelling.
- Exercises to strengthen the muscles in the shoulder and improve flexibility can restore shoulder movement and function.
- In some cases, corticosteroid injections may provide relief by reducing inflammation in the tendon.
Operative treatments
Surgery is generally considered if the non-surgical treatment options above fail to relieve symptoms or if there is significant weakness or deformity affecting daily activities. Surgery in patients under 50 usually involves reattaching the tendon to the humerus (upper arm bone), bypassing the injured area in the shoulder socket. The goal is to restore strength and reduce pain for improved functionality. In patients over 50 releasing the tendon in the shoulder without re-attachment is generally well tolerated and is a lower risk procedure, thanks to a second tendon that also holds the biceps tendon to the shoulder.
If surgery becomes necessary, Dr Lambers is here to help
If your GP determines that the surgical approach is worth considering, Dr Lambers will provide a plan and post-operative care to optimise shoulder function and prevent further injury.

