What causes ankle instability?
- An accident or fall that applies intense force to the ankle, such as landing on uneven ground from a height.
- Repeated mild injuries, such as ankle sprains, can lead to instability over time.
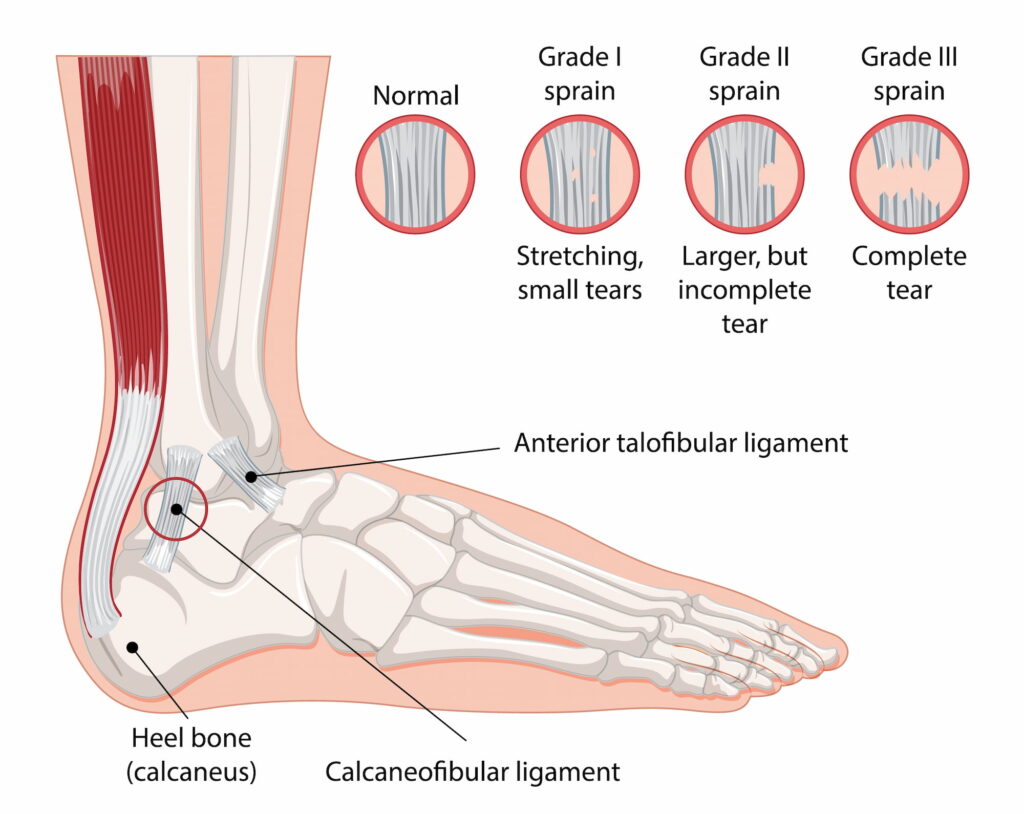
- Damage to the ligaments, particularly the anterior talofibular ligament (ATFL), is a common cause.
- Problems within the joint, such as loose bodies, avulsion fractures, or cartilage damage (osteochondral defects), may also be present.
What symptoms would I notice?
- Frequent situations where the ankle feels like it’s “giving way” or unreliable, leading to a lack of trust in its stability.
- Pain or clicking in the ankle, particularly at the front or back, worsened by activities like squatting.
- Recurrent ankle sprains
How is ankle instability diagnosed?
Your GP will provide an initial assessment of your ankle’s range of motion, stability, and areas of discomfort. This may require X-rays to check for fractures or bony abnormalities or an MRI for detailed images of ligament tears, cartilage issues or syndesmosis injury. If surgery is to be considered, your GP will refer you to Dr Lambers.
Treatment options
Ankle instability can be rectified with both non-operative and operative options. Almost all cases of ankle instability respond well to non-surgical methods, however surgery may be considered if frequent episodes occur despite a prolonged course of rehabilitation.
Non-operative treatments
- Strengthening exercises tailored to enhance ankle stability, especially focusing on proprioception exercises like balancing on one leg.
- Supportive braces or orthotic devices may be recommended to protect the ankle and reduce the risk of further injury.
- Avoiding high-impact activities and engaging in low-impact exercises can help reduce strain on the ankle.
- Over-the-counter pain relievers may assist with managing discomfort, particularly during rehabilitation.
Operative treatments
Lateral Ligament Reconstruction is the primary procedure performed to restore stability in the ankle joint by reconstructing the damaged ligaments. It may involve:
- Ankle arthroscopy to assess and treat internal joint issues before ligament repair.
- Ligament reconstruction in which the damaged ligament is reconstructed using the patient’s own tissue and sutures.
- For patients with hypermobility, surgical tape may reinforce the ligament.
- For patients with significant tissue loss from injury, or when instability occurs after a previous reconstruction, a tendon graft may be used to strengthen the repair.
Post-surgery, you will need to avoid weight-bearing on the affected ankle for about two weeks and will likely wear a CAM boot for support. With physiotherapy exercises you will gradually increase your range of motion, and a full recovery may take 6 months.
Read more about what ankle stabilisation surgery involves below:
Dr Lambers’ thorough evaluation to determine if surgery is required
If referred by your GP and surgery is offered, Dr Lambers will discuss the lateral ligament reconstruction process in detail to ensure you understand the procedure and recovery expectations. The goal is to restore ankle stability, reduce pain, and regain confidence in your movement, and Dr Lambers’ experience will help ensure this goal is reached.

