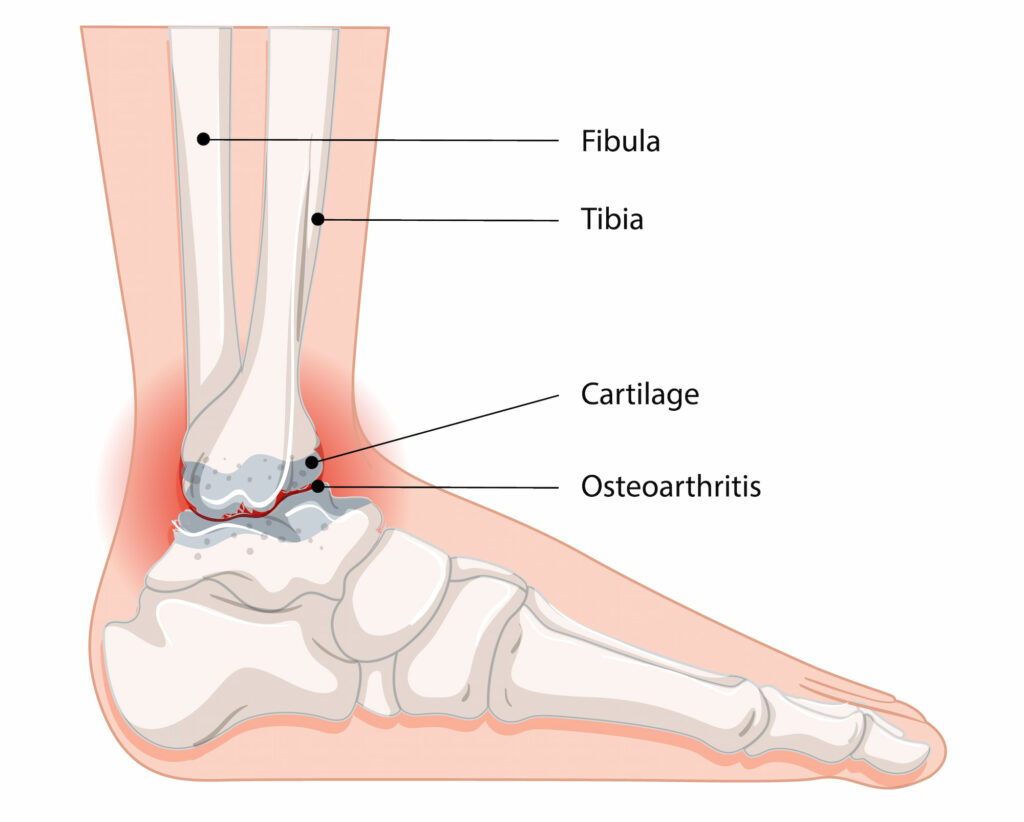
Ankle arthritis appears when the cartilage in the ankle joint deteriorates. Cartilage is crucial for smooth movement and acts as a cushion during weight-bearing activities. When arthritis sets in, the joint loses its normal shape, exposing the underlying bone and forming bony spurs, also known as osteophytes. This can cause pain and stiffness.
What causes ankle arthritis?
Ankle arthritis is most commonly caused by prior trauma, such as multiple ankle sprains or fractures, which can lead to post-traumatic arthritis. Over time, the wear associated with daily activities can also contribute to the condition. Other potential causes include osteoarthritis and inflammatory diseases like rheumatoid arthritis leading to joint inflammation and damage.
What symptoms would I notice?
Patients with ankle arthritis typically experience pain during activities like walking, and it can worsen to a constant ache throughout the day and even at night.
Other symptoms include:
- Swelling and warmth in the ankle
- Changes in foot or ankle shape
- Stiffness and decreased range of motion
How is ankle arthritis diagnosed?
The diagnosis of ankle arthritis starts with your GP, who will assess your ankle’s range of motion and check for signs of swelling or deformity. Standing X-rays are essential for accurately assessing the severity of arthritis, and an MRI may be used in the early stages when changes are not evident on X-rays, especially when evaluating soft tissue damage.
Treatment options for ankle arthritis
Treatment for ankle arthritis is dependent on the severity of the condition and your overall health and activity level.
Non-operative treatments
- Using an ankle brace can help stabilise the joint and reduce pain during activities.
- Cortisone injections may provide temporary relief by reducing inflammation.
- Over-the-counter medications to help manage pain.
- Reducing high-impact activities and incorporating low-impact exercises can alleviate symptoms.
- Exercises to strengthen the muscles around the ankle and work on your balance, improving stability and function.
- Custom shoes or insoles may be recommended to limit joint movement and provide support.
Operative treatments
Surgery is usually considered when non-surgical methods have failed to provide relief and the x-rays show advanced arthritis. Options include:
- A cheilectomy which involves removing bony spurs causing symptoms and is effective in specific cases called anterior ankle impingement syndrome.
- Ankle Fusion (Arthrodesis), often regarded as the “gold standard” for severe arthritis; a procedure that fuses the bones of the ankle joint, eliminating movement but providing significant pain relief. This is the most common procedure performed for ankle arthritis.
- Realignment Osteotomy which reshapes the bones around the joint to redistribute weight, preserving ankle motion. This is considered when the arthritis is in an earlier stage and confined to one side of the joint.
- Ankle Replacement, similar to hip and knee replacements, replacing the damaged ankle joint with an artificial joint to relieve pain while retaining some range of motion. This is considered in older patients particularly if there is arthritis in the joint below the ankle, the subtalar joint. Due to high rates of revision this surgery is not typically recommended in younger active individuals. Dr Lambers does not offer ankle replacement surgery but can refer you to a provider that does if it is deemed appropriate.
Read more about what ankle fusion entails or the post-operative recovery below:
Ankle arthritis surgery with Dr Lambers
Managing ankle arthritis involves a comprehensive approach tailored to your specific needs and lifestyle. While this starts with your GP, you may be referred to Dr Lambers to consider surgical treatment options.

