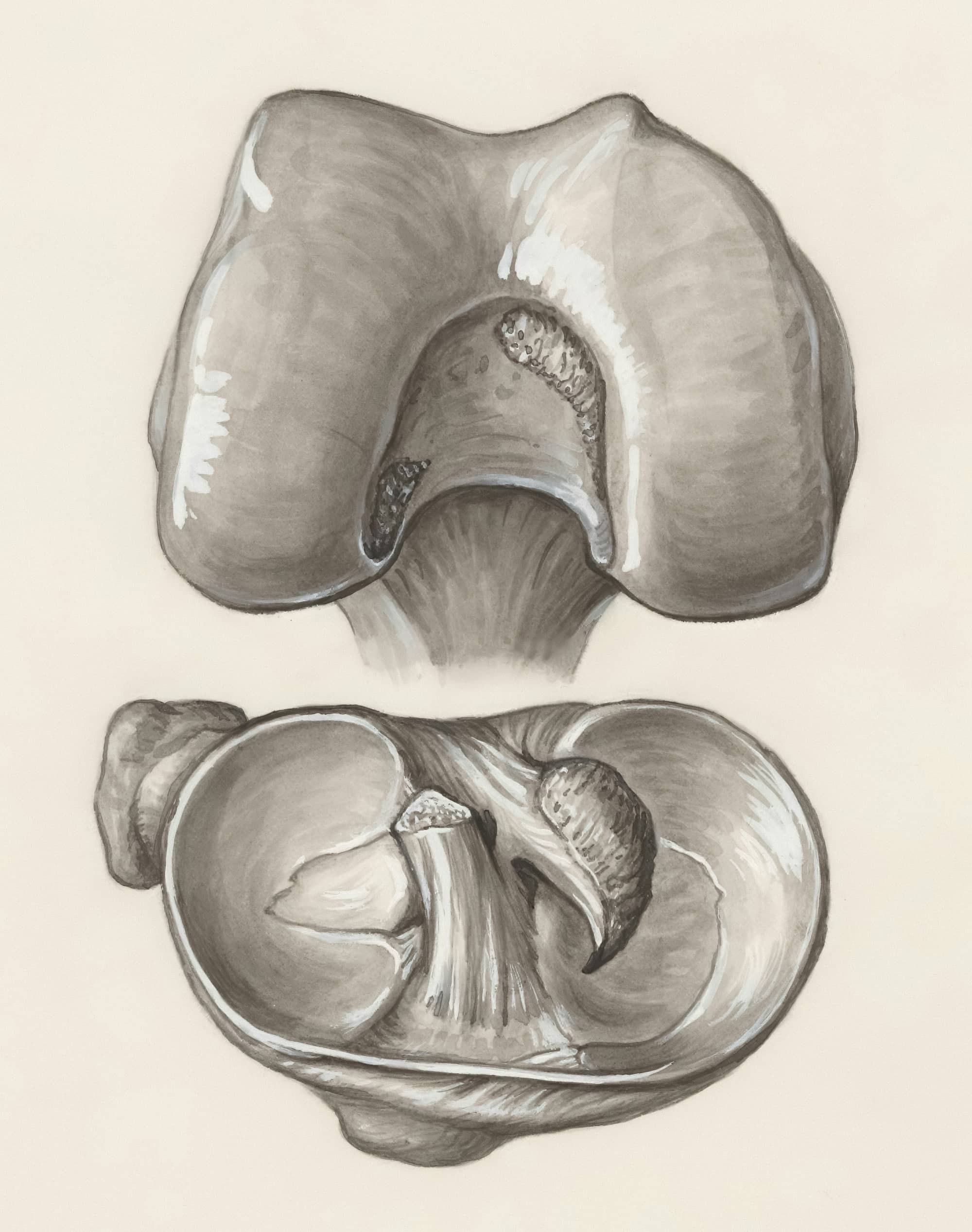
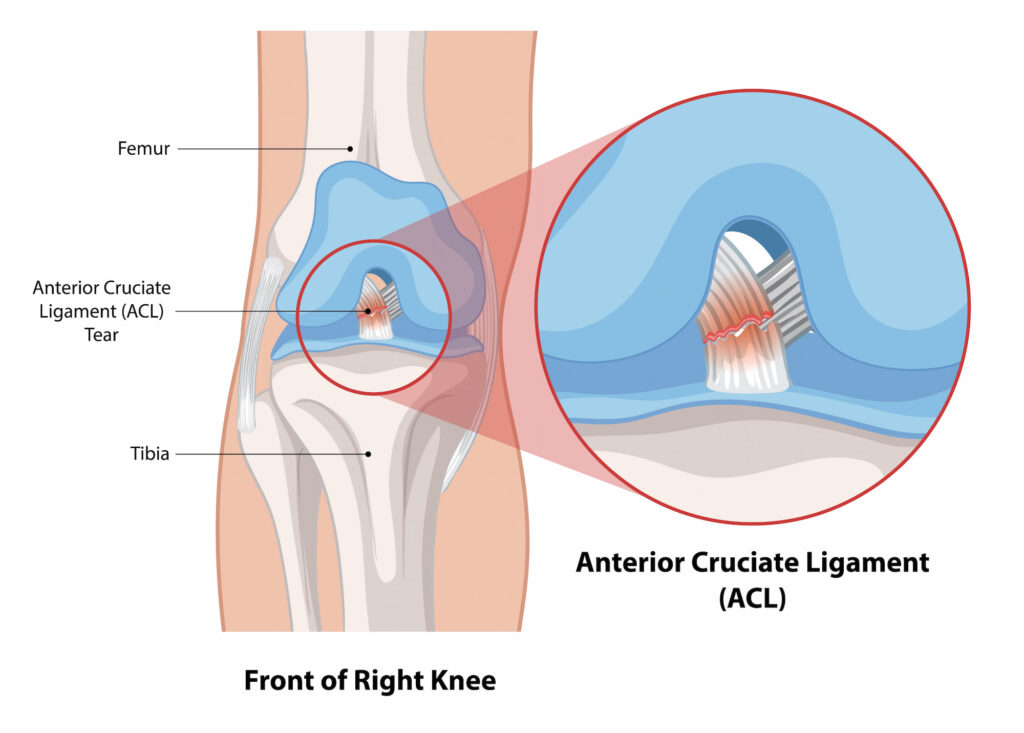
The ACL stretches diagonally across the knee, connecting the femur (thigh bone) to the tibia (shin bone), helping to control the forward movement of the tibia relative to the femur. ACL ruptures are common injuries, especially among athletes, and typically occur during activities that involve quick changes in direction, pivoting, or jumping.
What causes an ACL rupture?
ACL ruptures often occur during sports and activities that involve sudden stops, sharp pivots, or jumping, such as soccer, basketball, skiing, and football. Common causes include:
- Sudden directional changes or “cutting” with the foot planted
- Landing awkwardly from a jump
- Quickly decelerating while moving
- Direct impacts to the knee, such as those in a football tackle
In cases of severe trauma, the ACL may be rupture. Female athletes, in particular, face a higher risk of ACL injuries due to anatomical and hormonal factors.
Can I prevent an ACL rupture from occurring?
Warm up programs such as the FIFA11+ routine have been shown to reduce rates of ACL rupture thereby preventing some injuries. The FIFA 11+ program is a comprehensive warm-up routine developed by the FIFA Medical Assessment and Research Centre (F-MARC) to prevent injuries among soccer players, with a particular focus on reducing anterior cruciate ligament (ACL) injuries. Designed for players aged 14 and above, the program aims to enhance neuromuscular control, balance, and strength, thereby mitigating the risk of common soccer-related injuries such as ACL tears, hamstring strains, and ankle sprains. See below for a copy of the program.
What symptoms would I notice?
Symptoms of an ACL rupture are often immediate and intense, including:
- A loud pop or tearing sensation in the knee at the time of injury
- Rapid and significant swelling within hours
- Severe pain that makes it difficult to continue activity
- A feeling of instability or giving way when weight is put on the knee
- Limited range of motion, especially in flexing and extending the knee
If these symptoms are present and persist, or you experience instability or difficulty bearing weight, we recommend that you seek medical attention.
How is an ACL rupture diagnosed?
Your first step will be to see a GP who will take a complete medical history and conduct a physical examination. Imaging, such as:
- X-rays to rule out bone injuries or fractures
- MRI scans to visualise the ACL and assess the extent of soft tissue damage (which cannot be detected on an X-ray)
These diagnostic steps help confirm the rupture and determine the appropriate treatment pathway.
Treatment for an ACL rupture
Non-operative treatments
Non-operative treatments are suitable for older patients who don’t participate in pivot-heavy sports or activities. These treatments include:
- Physical therapy to strengthen knee muscles, improving stability and function
- Structured rehabilitation exercises to maintain range of motion and flexibility
- Supportive devices like braces for added stability during recovery
These treatments may be effective for patients who do not experience persistent knee instability. However, surgery remains an option if instability continues after rehabilitation.
Operative treatments
For younger patients or those engaged in sports with frequent directional changes, surgical treatment may be recommended:
- An ACL reconstruction is the primary surgical option, involving a graft (often from the patient’s hamstring, patellar tendon, or quadriceps tendon) to replace the torn ligament.
- LEAT (Lateral Extra-Articular Tenodesis) may be performed alongside reconstruction for added stability, especially in patients with a higher risk of instability and under 25 years old.
- In cases where both the MCL and ACL are injured, the MCL is typically treated in a brace or splint first, with ACL reconstruction following once range of motion is restored.
Read more about what ACL reconstruction surgery entails and the rehabilitaiton protocol afterwards:
Managing ACL ruptures with Dr Lambers
Dr Lambers emphasises non-operative management when suitable, such as in older adult patients, with a pathway to surgical intervention if non-operative treatments fail to achieve the desired stability. Surgery is typically recommended for young adults and adolescents. If your GP refers you to Dr Lambers, he will work with you to ensure you regain full knee function and confidence in your movement.