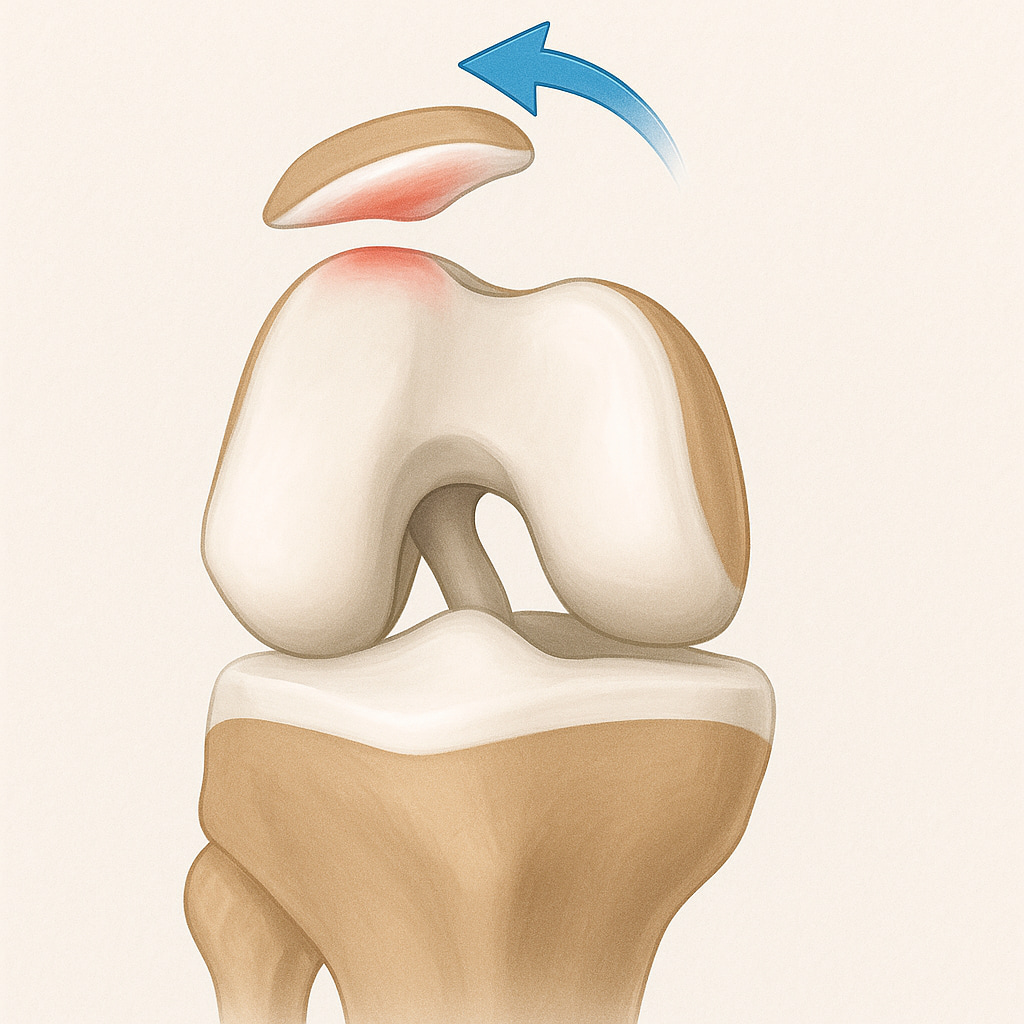
Patellofemoral joint (PFJ) instability is a condition affecting the knee joint, where the kneecap fails to maintain its proper position within the trochlear groove of the femur (thigh bone). This
can lead to dislocations or subluxations, causing pain and functional limitations.
PFJ instability can manifest as either traumatic dislocation, where the kneecap completely moves out of the groove, or chronic instability, where the kneecap partially dislocates (subluxation) but does not completely come out of place. PFJ instability often results from injury, overuse, or anatomical abnormalities and affects individuals of various ages, particularly those engaged in sports.
What causes PFJ instability?
- Sudden impacts or injuries to the knee can lead to a dislocated kneecap.
- Abnormalities in the shape of the femur, tibia, or patella, as well as variations in muscle strength or alignment, can predispose individuals to instability.
- Repetitive stress on the knee, particularly from sports involving jumping, running, or quick changes in direction, can contribute to instability.
- Weakness in the muscles around the knee, particularly the quadriceps, can lead to poor patellar tracking and an increased risk of dislocation.
What symptoms would I notice?
- A sensation of the kneecap shifting or dislocating during activity.
- Discomfort in and around the knee, especially during activities like climbing stairs or squatting.
- Inflammation around the knee joint, particularly after episodes of instability.
- A feeling of weakness or instability in the knee, causing difficulty walking or participating in sports.
- The knee may catch or lock due to loose fragments or misalignment of the patella.
How is PFJ instability diagnosed?
Your GP will assess your symptoms and examine you for knee stability, alignment, and range of motion using an X-ray to check for alignment issues and assess bone structures and potentially an MRI to evaluate soft tissues, cartilage, and ligaments for any injuries or damage.
Treatment options for PFJ instability
Most patients with PFJ instability respond well to non-surgical treatments; however, if non-operative treatments are ineffective, surgical options may be considered.
Non-operative treatments
- Targeted exercises to strengthen the quadriceps and other muscles around the knee to improve stability and function.
- A knee brace to support the joint during activities.
- Avoiding activities that exacerbate symptoms, especially high-impact sports.
- Applying ice and resting the knee to reduce swelling and pain.
Operative treatments
- The medial patellofemoral ligament (MPFL) can be reconstructed to provide better stability to the kneecap.
- Realignment procedures to correct bone alignment or shift the attachment of tendons and muscles to improve patellar tracking.
- Repositioning surgery of the insertion of the patellar tendon, called a tibial tubercle osteotomy, is considered if the kneecap sits too high or the tendon inserts in an abnormal position.
- A rare form of surgery called a trochleoplasty involves changing the depth of the groove on the femur that the kneecap slides in, however this is only required in a small group of patients.
See below for more information about the surgery for kneecap instability and some of the rehab protocols:
Managing PFJ instability with Dr Anton Lambers
In cases where surgical intervention is required, Dr Lambers will apply his experience to find the right solution for your needs. This, however, is only an option after a referral from your GP and non-surgical attempts to rectify the issue.

